Trauma
Category: Quickshot Oral Session 05
Quickshot Oral : Quickshot Oral Session 05
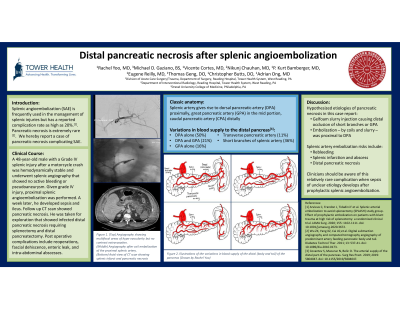
DISTAL PANCREATIC NECROSIS AFTER SPLENIC ANGIOEMBOLIZATION
Saturday, February 11, 2023
3:00pm - 4:00pm East Coast USA Time
Rachel Yoo, MD (she/her/hers)
General Surgery Resident PGY2
Reading Hospital, United States- AO
Adrian Ong, MD
Trauma Surgeon
Reading Hospital, United States
Presenter(s)
Principal Contact(s)
Objectives: Angioembolization (AE) of the spleen is a frequently used adjunct in the management of splenic injuries. While splenic ischemia or abscess is a well described complication, pancreatic necrosis is extremely rare. We hereby report a case of pancreatic necrosis complicating splenic AE.
A 48-year-old male was found to have a Grade IV splenic injury after a motor vehicle crash. As he was hemodynamically stable, he underwent splenic angiography which demonstrated no active bleeding or pseudoaneurysm. As this was a high-grade injury, the decision was made to perform main splenic artery embolization. One week later, he developed severe sepsis and ileus. Repeat CT imaging showed nonperfusion of the distal pancreas consistent with pancreatic necrosis. He underwent laparotomy with findings of necrosis of the distal pancreas comprising approximately 40% of the pancreas. Distal pancreatectomy was performed. He required multiple pancreatic debridements and endured a prolonged hospital course complicated by sepsis, acute respiratory failure, open abdomen with enteric leak, pulmonary embolism, and tracheal stenosis from prolonged tracheal intubation. He was eventually discharged after 6 weeks in the hospital. Review of the angiographic images showed that the embolization coils were deployed in the splenic artery proximal to the dorsal pancreatic artery thus resulting in ischemic pancreatic necrosis.
Pancreatic necrosis due to ischemia is an extremely rare complication that may result from proximal splenic artery embolization. Although splenic AE is a safe procedure with a low rate of complications requiring intervention, clinicians should have a high index of suspicion for ischemic complications after AE when sepsis of unclear etiology develops.
Methods:
Results:
Conclusion:
A 48-year-old male was found to have a Grade IV splenic injury after a motor vehicle crash. As he was hemodynamically stable, he underwent splenic angiography which demonstrated no active bleeding or pseudoaneurysm. As this was a high-grade injury, the decision was made to perform main splenic artery embolization. One week later, he developed severe sepsis and ileus. Repeat CT imaging showed nonperfusion of the distal pancreas consistent with pancreatic necrosis. He underwent laparotomy with findings of necrosis of the distal pancreas comprising approximately 40% of the pancreas. Distal pancreatectomy was performed. He required multiple pancreatic debridements and endured a prolonged hospital course complicated by sepsis, acute respiratory failure, open abdomen with enteric leak, pulmonary embolism, and tracheal stenosis from prolonged tracheal intubation. He was eventually discharged after 6 weeks in the hospital. Review of the angiographic images showed that the embolization coils were deployed in the splenic artery proximal to the dorsal pancreatic artery thus resulting in ischemic pancreatic necrosis.
Pancreatic necrosis due to ischemia is an extremely rare complication that may result from proximal splenic artery embolization. Although splenic AE is a safe procedure with a low rate of complications requiring intervention, clinicians should have a high index of suspicion for ischemic complications after AE when sepsis of unclear etiology develops.
Methods:
Results:
Conclusion:

