General Surgery
Category: Quickshot Oral Session 25
Quickshot Oral : Quickshot Oral Session 25
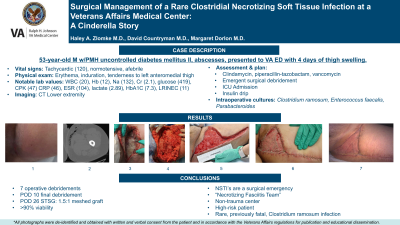
SURGICAL MANAGEMENT OF A RARE CLOSTRIDIAL NECROTIZING SOFT TISSUE INFECTION AT A VETERANS AFFAIRS MEDICAL CENTER: A CINDERELLA STORY
Tuesday, February 14, 2023
7:00am - 8:00am East Coast USA Time

Haley A. Zlomke, MD (she/her/hers)
Surgical Resident
Medical University of South Carolina, United States- MD
Margaret Dorlon, MD
United States
Presenter(s)
Principal Contact(s)
Objectives:
Introduction:
Necrotizing Soft Tissue Infections (NSTIs) portend a poor prognosis with significant morbidity and mortality. A previous report of a Clostridium ramosum NSTI proved fatal, however this case highlights the success in treating a rare and previously fatal condition in a patient with multiple risks factors.
Case Description:
A 53-year-old male with past medical history of uncontrolled Type 1 diabetes mellitus and MRSA abscesses presented to the emergency department after four days of left medial thigh swelling and erythema. He was normotensive, tachycardic and afebrile. He presented with a leukocytosis, hyperglycemic, hyponatremic with elevated creatinine, CRP, ESR and lactate. A CT scan showed extensive soft tissue gas tracking was seen along the medial thigh fascia. General Surgery was promptly consulted. Upon examination it was noted he had a small, 1 cm blister in his superior posteromedial thigh with significant edema, erythema, and induration. He was immediately started on broad spectrum antibiotics to include clindamycin, piperacillin-tazobactam, vancomycin and emergently taken to the operating room for debridement. Textbook, murky “dishwater” foul fluid was encountered tracking along the fascia and the debridement was carried until healthy tissue was reached. Aerobic and anaerobic cultures were sent for gram stain and culture. His wound was left open, packed with sodium hypochlorite solution and he was admitted to the ICU. He was started on an insulin drip to control his blood glucose and continued broad spectrum antibiotics. The cultures resulted in C. ramosum, E. Faecalis and Parabacteroides. He was taken back to the operating room for six additional debridements. He never became hemodynamically unstable. On post operative day 10 from index operation, he had his final debridement, and a negative pressure dressing was placed to his 32cm x 24cm x 5cm wound. Post operative day 26, he was deemed appropriate for autologous split thickness skin graft and a 1.5:1 meshed graft was used to cover the wound of 208 sq cm. His graft had >90% viability and has been seen in clinic with near complete healing of the skin graft.
Discussion:
NSTIs are a surgical emergency with some larger cities even implementing a “Necrotizing Fasciitis Team” due to the complex nature, resource intense and prolonged hospital stays for these patients. This was a remarkable case where prompt surgical intervention at a non-trauma center proved successful where previous literature highlighted the fatality of such a rare infection in a high-risk patient.
Methods:
Results:
Conclusion:
Introduction:
Necrotizing Soft Tissue Infections (NSTIs) portend a poor prognosis with significant morbidity and mortality. A previous report of a Clostridium ramosum NSTI proved fatal, however this case highlights the success in treating a rare and previously fatal condition in a patient with multiple risks factors.
Case Description:
A 53-year-old male with past medical history of uncontrolled Type 1 diabetes mellitus and MRSA abscesses presented to the emergency department after four days of left medial thigh swelling and erythema. He was normotensive, tachycardic and afebrile. He presented with a leukocytosis, hyperglycemic, hyponatremic with elevated creatinine, CRP, ESR and lactate. A CT scan showed extensive soft tissue gas tracking was seen along the medial thigh fascia. General Surgery was promptly consulted. Upon examination it was noted he had a small, 1 cm blister in his superior posteromedial thigh with significant edema, erythema, and induration. He was immediately started on broad spectrum antibiotics to include clindamycin, piperacillin-tazobactam, vancomycin and emergently taken to the operating room for debridement. Textbook, murky “dishwater” foul fluid was encountered tracking along the fascia and the debridement was carried until healthy tissue was reached. Aerobic and anaerobic cultures were sent for gram stain and culture. His wound was left open, packed with sodium hypochlorite solution and he was admitted to the ICU. He was started on an insulin drip to control his blood glucose and continued broad spectrum antibiotics. The cultures resulted in C. ramosum, E. Faecalis and Parabacteroides. He was taken back to the operating room for six additional debridements. He never became hemodynamically unstable. On post operative day 10 from index operation, he had his final debridement, and a negative pressure dressing was placed to his 32cm x 24cm x 5cm wound. Post operative day 26, he was deemed appropriate for autologous split thickness skin graft and a 1.5:1 meshed graft was used to cover the wound of 208 sq cm. His graft had >90% viability and has been seen in clinic with near complete healing of the skin graft.
Discussion:
NSTIs are a surgical emergency with some larger cities even implementing a “Necrotizing Fasciitis Team” due to the complex nature, resource intense and prolonged hospital stays for these patients. This was a remarkable case where prompt surgical intervention at a non-trauma center proved successful where previous literature highlighted the fatality of such a rare infection in a high-risk patient.
Methods:
Results:
Conclusion:

