Back
HPB
Category: Quickshot Oral Session 12
Quickshot Oral : Quickshot Oral Session 12
ANALYSIS OF PATIENT OUTCOMES AND FINANCIAL IMPLICATIONS OF READMISSIONS FOLLOWING ROBOTIC DISTAL PANCREATECTOMY AND SPLENECTOMY
Sunday, February 12, 2023
7:00am – 8:00am East Coast USA Time
- VB
Vincent Butano, MD (he/him/his)
Fellow
AdventHealth Tampa, United States - SR
Sharona Ross, MD
United States
Presenter(s)
Principal Contact(s)
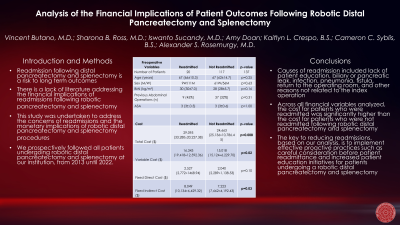
Objectives: The robotic platform for distal pancreatectomy and splenectomy has had exponential growth in recent years. Despite this growth, there is scarcity in the literature. The objective of this study is to identify amendable causes of readmissions following robotic distal pancreatectomy and splenectomy and to analyze the financial implications.
Methods: With IRB approval, we followed 137 patients following robotic distal pancreatectomy and splenectomy. Readmission was classified as rehospitalization within 30 days after patient operation. Total hospital cost includes patient initial and readmission hospital costs when applicable. The outcomes of patients were analyzed using Fisher’s exact test and Student’s t-test with significance assigned at p≤0.05. Data are presented as median (mean±SD).
Results: Of the 137 patients studied, 20 (15%) patients were readmitted within 30-days following discharge. Patients who were readmitted were 67 (66±10.3) years old, had a BMI of
30 (30±7.0) kg/m2, ASA of 3 (3±.0.5), with 9 (45%) having a previous abdominal operation. Comparatively, patients who were not readmitted were 67 (62±14.7) years old, had a BMI of 28 (28±5.7) kg/m2, ASA of 3 (3±.0.6), with 37 (32%) having a previous abdominal operation (p=NS, for all). Patients who were readmitted versus patients who were not had an operative duration of 327 (363±179.1) versus 251 (293±176.4) minutes (p=0.10), estimated blood loss (EBL) of 90 (159±214.6) versus 100 (244±559.4) mL (p=0.50), and a tumor size of 3 (4±2.0) versus 3 (4±2.9) cm (p=1.00). Patients who were readmitted versus patients who were not had a complication of Clavien-Dindo ≥III of 0 versus 5 (4%) (p=1.00), an initial hospital length of stay (LOS) of 5 (5±2.7) versus 4 (5±3.0) days (p=1.00), and a total hospital cost of $29,095 (33,280±20,227.38) versus $24,663 (25,136±10,786.45) (p=0.008).
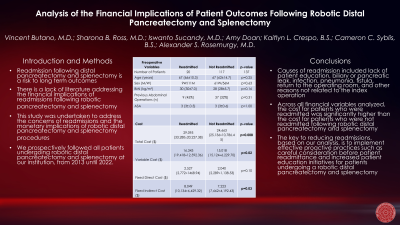
Conclusion: Patients were older and overweight with no preoperative differences between patients who were readmitted versus patients who were not. Patients who were readmitted had similar operative durations, EBL, tumor size, and LOS. Though a patient’s perioperative course may not differ, the fact of having a 30-day readmission increases the total hospital cost significantly. While complex operations are bound to produce readmissions in some capacity, we believe careful consideration before patient readmittance and increased patient education initiatives should be prioritized. These proactive actions would reduce patient readmissions and the increased financial burden placed upon the hospital and sequentially the patient.
Methods: With IRB approval, we followed 137 patients following robotic distal pancreatectomy and splenectomy. Readmission was classified as rehospitalization within 30 days after patient operation. Total hospital cost includes patient initial and readmission hospital costs when applicable. The outcomes of patients were analyzed using Fisher’s exact test and Student’s t-test with significance assigned at p≤0.05. Data are presented as median (mean±SD).
Results: Of the 137 patients studied, 20 (15%) patients were readmitted within 30-days following discharge. Patients who were readmitted were 67 (66±10.3) years old, had a BMI of
30 (30±7.0) kg/m2, ASA of 3 (3±.0.5), with 9 (45%) having a previous abdominal operation. Comparatively, patients who were not readmitted were 67 (62±14.7) years old, had a BMI of 28 (28±5.7) kg/m2, ASA of 3 (3±.0.6), with 37 (32%) having a previous abdominal operation (p=NS, for all). Patients who were readmitted versus patients who were not had an operative duration of 327 (363±179.1) versus 251 (293±176.4) minutes (p=0.10), estimated blood loss (EBL) of 90 (159±214.6) versus 100 (244±559.4) mL (p=0.50), and a tumor size of 3 (4±2.0) versus 3 (4±2.9) cm (p=1.00). Patients who were readmitted versus patients who were not had a complication of Clavien-Dindo ≥III of 0 versus 5 (4%) (p=1.00), an initial hospital length of stay (LOS) of 5 (5±2.7) versus 4 (5±3.0) days (p=1.00), and a total hospital cost of $29,095 (33,280±20,227.38) versus $24,663 (25,136±10,786.45) (p=0.008).
Conclusion: Patients were older and overweight with no preoperative differences between patients who were readmitted versus patients who were not. Patients who were readmitted had similar operative durations, EBL, tumor size, and LOS. Though a patient’s perioperative course may not differ, the fact of having a 30-day readmission increases the total hospital cost significantly. While complex operations are bound to produce readmissions in some capacity, we believe careful consideration before patient readmittance and increased patient education initiatives should be prioritized. These proactive actions would reduce patient readmissions and the increased financial burden placed upon the hospital and sequentially the patient.

