Back
HPB
Category: Quickshot Oral Session 02
Quickshot Oral : Quickshot Oral Session 02
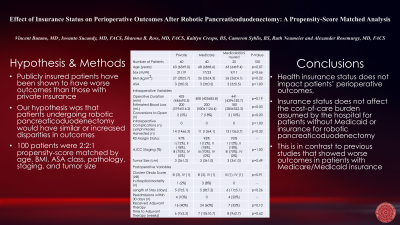
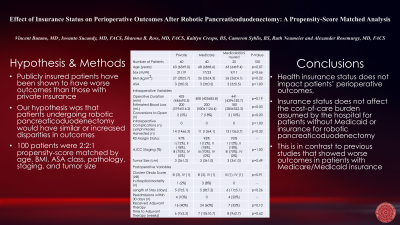
EFFECT OF INSURANCE STATUS ON PERIOPERATIVE OUTCOMES AFTER ROBOTIC PANCREATICODUODENECTOMY: A PROPENSITY-SCORE MATCHED ANALYSIS
Saturday, February 11, 2023
3:00pm – 4:00pm East Coast USA Time
- VB
Vincent Butano, MD (he/him/his)
Fellow
AdventHealth Tampa, United States - SR
Sharona Ross, MD
United States
Presenter(s)
Principal Contact(s)
Objectives: The effect of having Medicaid or being uninsured is thought to negatively impact a patient’s postoperative course, yet little has been published to support this claim. This study was undertaken to determine the impact of insurance status on perioperative outcomes in patients undergoing robotic pancreaticoduodenectomy.
Methods: With IRB approval, we prospectively follow 364 patients who underwent robotic pancreaticoduodenectomy. Patients were stratified by their health insurance (i.e., Private, Medicare, and Medicaid/Uninsured); 100 patients were 2:2:1 propensity-score matched by age, BMI, ASA class, pathology, 8th edition AJCC staging, and tumor size. Perioperative variables were compared utilizing contingency testing and an ANOVA of repeated measures. Statistical significance was accepted at a p-value≤0.05 and the data are presented as median (mean±SD).
Results: The 100 patients undergoing propensity-score matching were 64 (65±9.1) years old with a BMI of 27 (27±4.9) kg/m2 and ASA class of 3 (3±0.5). Operative duration was 421 (428±105.9) minutes and estimated blood loss was 200 (385±795.0) mL. There were 4 in-hospital deaths and 8 readmissions within 30 days of discharge. Total hospital cost was $32,064 (38,014±22,205.94).
After matching, no differences were found in pre-, intra-, and short-term postoperative variables among patients with different types of insurance, including hospital cost and time to initiation of adjuvant treatment, which was 8 (9±7.9) weeks, for patients with malignant disease (Table).
Conclusion: In our hepatopancreaticobiliary program, health insurance status does not impact patients’ perioperative outcomes, nor does it affect the cost-of-care burden assumed by the hospital for patients without Medicaid or insurance for robotic pancreaticoduodenectomy.
Methods: With IRB approval, we prospectively follow 364 patients who underwent robotic pancreaticoduodenectomy. Patients were stratified by their health insurance (i.e., Private, Medicare, and Medicaid/Uninsured); 100 patients were 2:2:1 propensity-score matched by age, BMI, ASA class, pathology, 8th edition AJCC staging, and tumor size. Perioperative variables were compared utilizing contingency testing and an ANOVA of repeated measures. Statistical significance was accepted at a p-value≤0.05 and the data are presented as median (mean±SD).
Results: The 100 patients undergoing propensity-score matching were 64 (65±9.1) years old with a BMI of 27 (27±4.9) kg/m2 and ASA class of 3 (3±0.5). Operative duration was 421 (428±105.9) minutes and estimated blood loss was 200 (385±795.0) mL. There were 4 in-hospital deaths and 8 readmissions within 30 days of discharge. Total hospital cost was $32,064 (38,014±22,205.94).
After matching, no differences were found in pre-, intra-, and short-term postoperative variables among patients with different types of insurance, including hospital cost and time to initiation of adjuvant treatment, which was 8 (9±7.9) weeks, for patients with malignant disease (Table).
Conclusion: In our hepatopancreaticobiliary program, health insurance status does not impact patients’ perioperative outcomes, nor does it affect the cost-of-care burden assumed by the hospital for patients without Medicaid or insurance for robotic pancreaticoduodenectomy.

