Back
Vascular
Category: Quickshot Oral Session 16
Quickshot Oral : Quickshot Oral Session 16
INFERIOR VENA CAVA FILTER OCCLUSION CAUSING PHLEGMASIA ALBA DOLENS
Monday, February 13, 2023
7:00am – 8:00am East Coast USA Time

Jeremy Burt, MD
General Surgery Resident, PGY-1
University of Mississippi Medical Center, United States- MM
Marc E. Mitchell, MD
United States
Presenter(s)
Principal Contact(s)
Objectives:
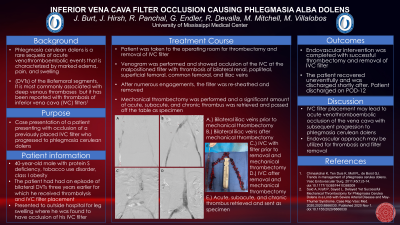
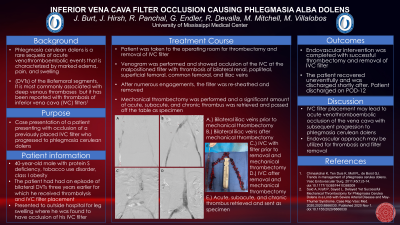
Background: Phlegmasia alba dolens is a rare sequela of acute extensive venothrombus of the iliofemoral segments characterized by marked edema, pain, and swelling. Due to total occlusion of the deep venous system, outflow relies on the superficial system for drainage. Once the superficial system also becomes impaired, there is complete outflow obstruction impeding arterial inflow and increasing risk of gangrene, i.e. phegmasia cerulean dolens. Rarely, phlegmasia albla doens can also result from clotted inferior vena cava (IVC) filter. Given such devastating consequences, early recognition and treatment of this condition is vital.
Methods: A 39-year-old truck driver with protein S deficiency, tobacco use disorder, class I obesity, and prior inferior vena cava (IVC) filter placement after remote trauma presented to the emergency department with progressive bilateral lower extremity pain and swelling. The patient had previously completed a 6 month oral anticoagulation treatment course. Venous duplex revealed extensive bilateral deep vein thromboses (DVTs) from the external iliac veins to popliteal veins, as well as, thrombophlebitis of the left great saphenous vein. Vascular Surgery was consulted for evaluation and treatment.
Results: Given the risk of progression to phlegmasia cerulean dolens and development of post thrombotic syndrome - urgent endovascular thrombectomy was offered. Venography confirmed patency of the suprarenal vena cava with abrupt occlusion of the infrarenal segment at the level of the malpositioned IVC filter. Complete thrombotic occlusion was seen down to the bilateral popliteal veins. Using a 20 Fr GORE® DrySeal Flex Introducer Sheath (W. L. Gore & Associates, Inc.) via the right internal jugular as a stable platform, the filter was engaged using wire loop technique and directed into the access sheath using a daughtered Medtronic TourGuide™ steerable 8.5F sheath and successfully removed. This was followed by endovascular thrombectomy using the Inari ClotTriever® system to debulk the IVC and bilateral iliofemoral segments. Adjunctive venoplasty with a DORADO® PTA catheter (Bard Medical, Covington, GA) used to soften mild venous irregularities, while intravascular ultrasound confirmed patency and excluded extrinsic compression. A staged approach was utilized for the bilateral femoral popliteal segments via popliteal access. The patient progressed well with rapid resolution of symptoms and discharged on therapeutic dose ELIQUIS®.
Conclusion: IVC filter placement may lead to thrombotic occlusion of the vena cava with subsequent progression to phlegmasia alba dolens. A staged endovascular approach may be utilized for acute on chronic caval thrombosis and filter removal.
Methods:
Results:
Conclusion:
Background: Phlegmasia alba dolens is a rare sequela of acute extensive venothrombus of the iliofemoral segments characterized by marked edema, pain, and swelling. Due to total occlusion of the deep venous system, outflow relies on the superficial system for drainage. Once the superficial system also becomes impaired, there is complete outflow obstruction impeding arterial inflow and increasing risk of gangrene, i.e. phegmasia cerulean dolens. Rarely, phlegmasia albla doens can also result from clotted inferior vena cava (IVC) filter. Given such devastating consequences, early recognition and treatment of this condition is vital.
Methods: A 39-year-old truck driver with protein S deficiency, tobacco use disorder, class I obesity, and prior inferior vena cava (IVC) filter placement after remote trauma presented to the emergency department with progressive bilateral lower extremity pain and swelling. The patient had previously completed a 6 month oral anticoagulation treatment course. Venous duplex revealed extensive bilateral deep vein thromboses (DVTs) from the external iliac veins to popliteal veins, as well as, thrombophlebitis of the left great saphenous vein. Vascular Surgery was consulted for evaluation and treatment.
Results: Given the risk of progression to phlegmasia cerulean dolens and development of post thrombotic syndrome - urgent endovascular thrombectomy was offered. Venography confirmed patency of the suprarenal vena cava with abrupt occlusion of the infrarenal segment at the level of the malpositioned IVC filter. Complete thrombotic occlusion was seen down to the bilateral popliteal veins. Using a 20 Fr GORE® DrySeal Flex Introducer Sheath (W. L. Gore & Associates, Inc.) via the right internal jugular as a stable platform, the filter was engaged using wire loop technique and directed into the access sheath using a daughtered Medtronic TourGuide™ steerable 8.5F sheath and successfully removed. This was followed by endovascular thrombectomy using the Inari ClotTriever® system to debulk the IVC and bilateral iliofemoral segments. Adjunctive venoplasty with a DORADO® PTA catheter (Bard Medical, Covington, GA) used to soften mild venous irregularities, while intravascular ultrasound confirmed patency and excluded extrinsic compression. A staged approach was utilized for the bilateral femoral popliteal segments via popliteal access. The patient progressed well with rapid resolution of symptoms and discharged on therapeutic dose ELIQUIS®.
Conclusion: IVC filter placement may lead to thrombotic occlusion of the vena cava with subsequent progression to phlegmasia alba dolens. A staged endovascular approach may be utilized for acute on chronic caval thrombosis and filter removal.
Methods:
Results:
Conclusion:

