Pediatrics
Category: Quickshot Oral Session 26
Quickshot Oral : Quickshot Oral Session 26
DOES PRESENTING FACILITY AND RACE IMPACT OUTCOMES AND MANAGEMENT OF PYLORIC STNEOSIS
Tuesday, February 14, 2023
7:00am - 8:00am East Coast USA Time
- CN
Cory Nonnemacher, MD
United States
- CN
Cory Nonnemacher, MD
United States
Presenter(s)
Principal Contact(s)
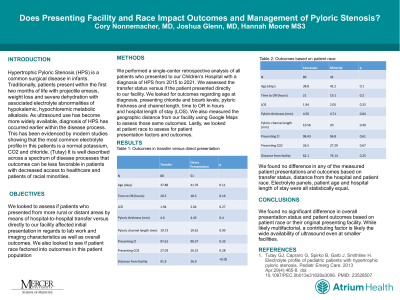
Objectives: Hypertrophic Pyloric Stenosis (HPS) is a common surgical disease in infants. Traditionally, patients present with projectile emesis, weight loss and severe dehydration with associated electrolyte abnormalities of hypokalemic, hypochloremic metabolic alkalosis. As ultrasound use has become more widely available, diagnosis of HPS has occurred earlier within the disease process. We looked to assess if patients presenting as a transfer versus directly to a facility with pediatric surgical capabilities affected patients' initial presentation and overall outcomes. Many adult and pediatric disease processes show a discrepancy in outcomes based on race and we looked to assess if this is present in HPS.
Methods: We performed a retrospective analysis of all patients who presented to our Children’s Hospital with a diagnosis of HPS from 2015 to 2021. We looked at how geographic distance from our facility, transfer status and patient race affected patients presenting chloride level, bicarb level and hospital length of stay (LOS).
Results: 131 patients presented to our facility with HPS, 80 via transfer and 51 as a direct presentation from 2015 to 2021. All were managed surgically with a laparoscopic pyloromyotomy with no negative laparoscopies performed. We found no statistically significant difference in patients’ presenting Cl levels, CO2 levels and hospital LOS in those transferred versus those that presented directly. We also found no differences in these variables based on patient race. Lastly, we performed Spearman’s rank-order correlation and found no statistical correlation between total miles in distance travelled for care and patient presenting laboratory work and outcomes.
Conclusion: We found no significant differences in overall presentation and outcomes based on patient race, transfer status or geographical location. We believe this reflects an evolution in the advancement and availability of ultrasound use and standardization on management of hypertrophic pyloric stenosis. We suggest that this could be used as a model for standardizing care to equalize outcomes in other pediatric diseases which currently show large disparities in care based on race and geographical location.
Methods: We performed a retrospective analysis of all patients who presented to our Children’s Hospital with a diagnosis of HPS from 2015 to 2021. We looked at how geographic distance from our facility, transfer status and patient race affected patients presenting chloride level, bicarb level and hospital length of stay (LOS).
Results: 131 patients presented to our facility with HPS, 80 via transfer and 51 as a direct presentation from 2015 to 2021. All were managed surgically with a laparoscopic pyloromyotomy with no negative laparoscopies performed. We found no statistically significant difference in patients’ presenting Cl levels, CO2 levels and hospital LOS in those transferred versus those that presented directly. We also found no differences in these variables based on patient race. Lastly, we performed Spearman’s rank-order correlation and found no statistical correlation between total miles in distance travelled for care and patient presenting laboratory work and outcomes.
Conclusion: We found no significant differences in overall presentation and outcomes based on patient race, transfer status or geographical location. We believe this reflects an evolution in the advancement and availability of ultrasound use and standardization on management of hypertrophic pyloric stenosis. We suggest that this could be used as a model for standardizing care to equalize outcomes in other pediatric diseases which currently show large disparities in care based on race and geographical location.

