General Surgery
Category: Quickshot Oral Session 19
Quickshot Oral : Quickshot Oral Session 19
RETROGRADE JEJUNOGASTRIC INTUSUSSCEPTION OF EFFERENT LIMB POST WHIPPLE'S PROCEDURE
Monday, February 13, 2023
7:00am - 8:00am East Coast USA Time
- JN
Jacqueline Nguyen Khuong, MD
United States
- JN
Jacqueline Nguyen Khuong, MD
United States
Presenter(s)
Principal Contact(s)
Objectives: Jejunogastric intussusception (JGI) is a rare but potentially life-threatening complication of gastric surgery with an incidence of < 0.1%. We present two cases of JGI in patients who had undergone a Whipple’s procedure.
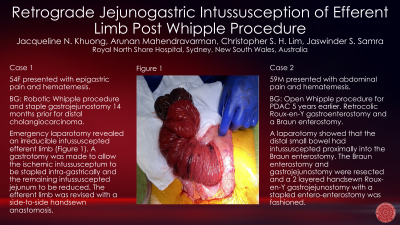
The first case is of a 54-year-old female who presented to the emergency department with worsening epigastric pain on a background of a two-month history of intermittent epigastric pain with associated nausea and vomiting. She underwent a robotic Whipple’s procedure with stapled gastrojejunostomy 14 months prior for a distal cholangiocarcinoma. An urgent gastroscopy was performed after she developed haematemesis during her admission, which revealed a long segment of prolapsing jejunum from the gastrojejunostomy with evidence of mucosal ischaemia. A midline laparotomy was performed which revealed that the intussuscepted segment was her efferent limb; this was unable to be reduced with gentle traction. A gastrostomy was made to allow access to the intussusceptum, which measured 60cm and to staple the ischaemic intussusceptum intragastrically. This allowed the remaining intussuscepted jejunum to be reduced. After reduction, the efferent limb was revised with a side-to-side handsewn anastomosis. Histopathology of the resected segment showed ischaemic changes but no cause for a potential lead point as the cause of the intussusception.
The second case is a 59-year-old male with 2 weeks of generalised abdominal pain and an episode of haematemesis after a Whipple's procedure for PDAC 5 years earlier and adjuvant chemotherapy. He developed recurrence in the lung and remnant pancreas in 2019 and was enrolled in a chemotherapy trial with good response. His reconstruction at the time of his Whipple's was a retrocolic roux-en-Y gastroenterostomy and a Braun enterostomy. CT showed a segment of small bowel intussusception, at the small bowel anastomosis in the left hemiabdomen, with upstream luminal distension. An urgent gastroscopy showed ulceration and necrosis in both limbs of the gastrojejunostomy and a laparotomy was performed. This showed that the distal small bowel had intussuscepted proximally into the Braun entero-enterostomy. The Braun enterostomy and gastrojejunostomy was resected and a 2 layered handsewn roux-en-Y gastrojejunostomy with a stapled enteroenterostomy was fashioned.
JGI is a rare but critical diagnosis and should be considered in all patients with gastric surgical anastomosis. The management of acute JGI involves resuscitation and urgent operative reduction. Surgical approach to JGI typically involves manual reduction, resection of affected bowel, and revision of anastomosis with consideration of fixation to neighbouring structures to prevent recurrence.
Methods:
Results:
Conclusion:
The first case is of a 54-year-old female who presented to the emergency department with worsening epigastric pain on a background of a two-month history of intermittent epigastric pain with associated nausea and vomiting. She underwent a robotic Whipple’s procedure with stapled gastrojejunostomy 14 months prior for a distal cholangiocarcinoma. An urgent gastroscopy was performed after she developed haematemesis during her admission, which revealed a long segment of prolapsing jejunum from the gastrojejunostomy with evidence of mucosal ischaemia. A midline laparotomy was performed which revealed that the intussuscepted segment was her efferent limb; this was unable to be reduced with gentle traction. A gastrostomy was made to allow access to the intussusceptum, which measured 60cm and to staple the ischaemic intussusceptum intragastrically. This allowed the remaining intussuscepted jejunum to be reduced. After reduction, the efferent limb was revised with a side-to-side handsewn anastomosis. Histopathology of the resected segment showed ischaemic changes but no cause for a potential lead point as the cause of the intussusception.
The second case is a 59-year-old male with 2 weeks of generalised abdominal pain and an episode of haematemesis after a Whipple's procedure for PDAC 5 years earlier and adjuvant chemotherapy. He developed recurrence in the lung and remnant pancreas in 2019 and was enrolled in a chemotherapy trial with good response. His reconstruction at the time of his Whipple's was a retrocolic roux-en-Y gastroenterostomy and a Braun enterostomy. CT showed a segment of small bowel intussusception, at the small bowel anastomosis in the left hemiabdomen, with upstream luminal distension. An urgent gastroscopy showed ulceration and necrosis in both limbs of the gastrojejunostomy and a laparotomy was performed. This showed that the distal small bowel had intussuscepted proximally into the Braun entero-enterostomy. The Braun enterostomy and gastrojejunostomy was resected and a 2 layered handsewn roux-en-Y gastrojejunostomy with a stapled enteroenterostomy was fashioned.
JGI is a rare but critical diagnosis and should be considered in all patients with gastric surgical anastomosis. The management of acute JGI involves resuscitation and urgent operative reduction. Surgical approach to JGI typically involves manual reduction, resection of affected bowel, and revision of anastomosis with consideration of fixation to neighbouring structures to prevent recurrence.
Methods:
Results:
Conclusion:

