Back
Vascular
Category: Quickshot Oral Session 17
Quickshot Oral : Quickshot Oral Session 17
RUPTURED POPLITEAL ARTERY ANEURYSM: A CASE REPORT
Monday, February 13, 2023
7:00am – 8:00am East Coast USA Time

Sigrid Williamson, MD
Resident
Reading Hospital, United States- hZ
hong Zheng, DO
United States
Presenter(s)
Principal Contact(s)
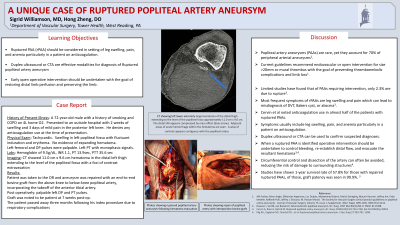
Objectives: Popliteal artery aneurysms (PAAs) are rare amongst the general population and are typically complicated by thrombosis or distal embolization1. Ruptured popliteal artery aneurysms (rPAAs) are exceedingly rare and have been noted as being associated with anticoagulation7. We present the case of a spontaneous rPAA.
A 72-year-old male presented with 2 weeks of worsening posterior left knee swelling and pain. The patient had COPD and a remote smoking history. On exam, there was swelling in the left popliteal fossa with fluctuant induration and erythema. Left femoral and DP pulses were palpable with a monophasic left PT signal. He was tachycardic with a hemoglobin of 9.5 and normal coagulation studies. A CT scan showed an 11.0 cm x 9.6 cm hematoma in the distal left thigh extending to the popliteal fossa with foci of contrast extravasation. The patient was taken to the operating room and the popliteal fossa was explored. A large hematoma was noted overlying a ruptured saccular aneurysm (Figure 1). The aneurysm was repaired with an end-to-end bovine graft from the above-knee to the below-knee popliteal artery. At the conclusion of the case, the patient had palpable left DP and PT pulse.
Popliteal artery aneurysms (PAAs) account for 70% of peripheral arterial aneurysms2. Current guidelines recommend intervention for size >20mm or presence of mural thrombus with the goal of preventing thromboembolic complications and limb loss1. Rupture of PAAs is exceedingly rare with incidence of about 2.3% 7, 8. Due to the rarity of ruptured PAAs there is a paucity of data regarding presentation, management, and outcomes. Symptoms of rPAAs are often related to compression of adjacent structures and vasculature. Studies have implicated anticoagulation use in nearly half of the incidents of rPAAs7. No guidelines currently exist regarding the treatment of rPAAs. However, when identified, operative intervention should be undertaken to control bleeding, re-establish distal flow, and evacuate the resultant hematoma7,8. Posterior popliteal incision provides excellent exposure for hematoma evacuation and in-situ arterial reconstruction. Circumferential control and dissection of the artery can often be avoided, reducing the risk of damage to surrounding structures8. Cervin et al saw 1-year survival rate of 57.8% for those with repaired ruptured PAAs, of those, graft patency was seen in 90.9%. Our patient was noted to have a patent graft at seven-week follow-up. However, he passed away three months following his index procedure due to respiratory complications.
Methods:
Results:
Conclusion:
A 72-year-old male presented with 2 weeks of worsening posterior left knee swelling and pain. The patient had COPD and a remote smoking history. On exam, there was swelling in the left popliteal fossa with fluctuant induration and erythema. Left femoral and DP pulses were palpable with a monophasic left PT signal. He was tachycardic with a hemoglobin of 9.5 and normal coagulation studies. A CT scan showed an 11.0 cm x 9.6 cm hematoma in the distal left thigh extending to the popliteal fossa with foci of contrast extravasation. The patient was taken to the operating room and the popliteal fossa was explored. A large hematoma was noted overlying a ruptured saccular aneurysm (Figure 1). The aneurysm was repaired with an end-to-end bovine graft from the above-knee to the below-knee popliteal artery. At the conclusion of the case, the patient had palpable left DP and PT pulse.
Popliteal artery aneurysms (PAAs) account for 70% of peripheral arterial aneurysms2. Current guidelines recommend intervention for size >20mm or presence of mural thrombus with the goal of preventing thromboembolic complications and limb loss1. Rupture of PAAs is exceedingly rare with incidence of about 2.3% 7, 8. Due to the rarity of ruptured PAAs there is a paucity of data regarding presentation, management, and outcomes. Symptoms of rPAAs are often related to compression of adjacent structures and vasculature. Studies have implicated anticoagulation use in nearly half of the incidents of rPAAs7. No guidelines currently exist regarding the treatment of rPAAs. However, when identified, operative intervention should be undertaken to control bleeding, re-establish distal flow, and evacuate the resultant hematoma7,8. Posterior popliteal incision provides excellent exposure for hematoma evacuation and in-situ arterial reconstruction. Circumferential control and dissection of the artery can often be avoided, reducing the risk of damage to surrounding structures8. Cervin et al saw 1-year survival rate of 57.8% for those with repaired ruptured PAAs, of those, graft patency was seen in 90.9%. Our patient was noted to have a patent graft at seven-week follow-up. However, he passed away three months following his index procedure due to respiratory complications.
Methods:
Results:
Conclusion:

