Back
GI
Category: Quickshot Oral Session 21
Quickshot Oral : Quickshot Oral Session 21
SMALL BOWEL OBSTRUCTION SECONDARY TO RARE DUODENAL DIVERTICULITIS WITH ENTEROLITH FORMATION
Monday, February 13, 2023
7:00am – 8:00am East Coast USA Time

Clive J. Miranda, DO
Resident
University at Buffalo
Buffalo, New York, United States- MA
Matthew V. Akbar, MD
Medical Student
University at Buffalo, United States
Presenter(s)
Co-Author(s)
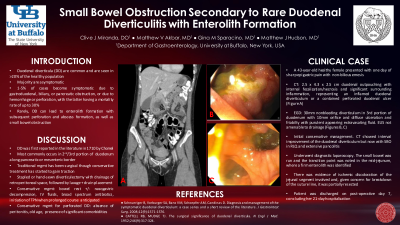
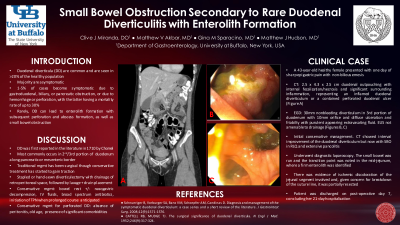
Objectives: Duodenal diverticula (DD) are relatively common and are seen in over 20% of the healthy population. The vast majority are asymptomatic and discovered incidentally on imaging. However, 1-5% of cases become symptomatic due to gastroduodenal, biliary, or pancreatic obstruction, or due to hemorrhage or perforation, with the latter having a mortality rate of up to 30%. In very rare cases, DD can lead to enterolith formation with subsequent perforation and abscess formation, as well as small bowel obstruction in that region or distally. We present a case of a middle-aged female with inflammation and ulceration of a duodenal diverticulum along with enterolith formation that impacted distally in the jejunum leading to a small bowel obstruction.
A 43-year-old healthy female presented with one day of sharp epigastric abdominal pain accompanied by non-bilious emesis with subjective fevers. Computed tomography showed a 2.5 x 4.3 x 2.5 cm duodenal outpouching with internal fecalization/necrosis and significant surrounding inflammation, representing an inflamed duodenal diverticulum or a contained perforated duodenal ulcer. Upper endoscopy revealed a 30mm nonbleeding diverticulum in the third portion of the duodenum with a 10mm orifice and evidence of diffuse ulceration and friability with purulent appearing extravasating fluid. Endosonographic findings revealed a 4-cm heterogenous collection cephalad to the diverticulum which was not amenable for endoscopic drainage. The patient was managed conservatively with antibiotics. Two days post-endoscopy, she developed abdominal pain again with bilious emesis. CT showed interval improvement of the duodenal diverticulum but now with small bowel obstruction with a transition point in the right lower quadrant and development of extensive pancolitis. The patient underwent a diagnostic laparoscopy. The small bowel was run and the transition point was noted in the mid-jejunum, where a firm enterolith was identified. There was evidence of ischemic discoloration of the jejunal segment involved and, given concern for breakdown of the suture line, it was partially resected. The patient’s post-operative course was uncomplicated and she was discharged on post-operative day 7, concluding her 21-day hospitalization.
Inflammation with enterolith formation leading to small bowel obstruction is an exceedingly rare complication of duodenal diverticula with only a handful of cases reported in the literature. Though the traditional treatment method has been surgical, there have been cases of conservative management leading to favorable outcomes. Our case highlights a very interesting complication of duodenal diverticula and aims to educate clinicians on prompt recognition and management of this uncommon phenomenon.
Methods:
Results:
Conclusion:
A 43-year-old healthy female presented with one day of sharp epigastric abdominal pain accompanied by non-bilious emesis with subjective fevers. Computed tomography showed a 2.5 x 4.3 x 2.5 cm duodenal outpouching with internal fecalization/necrosis and significant surrounding inflammation, representing an inflamed duodenal diverticulum or a contained perforated duodenal ulcer. Upper endoscopy revealed a 30mm nonbleeding diverticulum in the third portion of the duodenum with a 10mm orifice and evidence of diffuse ulceration and friability with purulent appearing extravasating fluid. Endosonographic findings revealed a 4-cm heterogenous collection cephalad to the diverticulum which was not amenable for endoscopic drainage. The patient was managed conservatively with antibiotics. Two days post-endoscopy, she developed abdominal pain again with bilious emesis. CT showed interval improvement of the duodenal diverticulum but now with small bowel obstruction with a transition point in the right lower quadrant and development of extensive pancolitis. The patient underwent a diagnostic laparoscopy. The small bowel was run and the transition point was noted in the mid-jejunum, where a firm enterolith was identified. There was evidence of ischemic discoloration of the jejunal segment involved and, given concern for breakdown of the suture line, it was partially resected. The patient’s post-operative course was uncomplicated and she was discharged on post-operative day 7, concluding her 21-day hospitalization.
Inflammation with enterolith formation leading to small bowel obstruction is an exceedingly rare complication of duodenal diverticula with only a handful of cases reported in the literature. Though the traditional treatment method has been surgical, there have been cases of conservative management leading to favorable outcomes. Our case highlights a very interesting complication of duodenal diverticula and aims to educate clinicians on prompt recognition and management of this uncommon phenomenon.
Methods:
Results:
Conclusion:

