Breast
Category: Quickshot Oral Session 01
Quickshot Oral : Quickshot Oral Session 01
POSITIVE NIPPLE MARGINS AND ONCOLOGIC OUTCOMES OF NIPPLE-SPARING MASTECTOMY IN A LARGE COMMUNITY-BASED HOSPITAL SYSTEM
Saturday, February 11, 2023
3:00pm - 4:00pm East Coast USA Time
- KS
Kristina Shaffer, MD
Breast Surgical Oncologist
Novant Health, United States - KS
Kristina Shaffer, MD
Breast Surgical Oncologist
Novant Health, United States
Presenter(s)
Principal Contact(s)
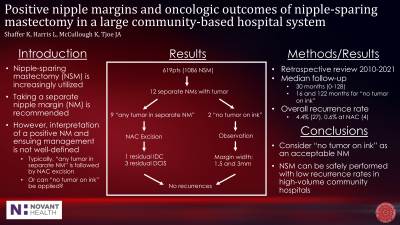
Objectives: Current guidelines regarding nipple-sparing mastectomy (NSM), including the American Society of Breast Surgeons, emphasize the importance of sending a separate nipple margin, but do not specifically define what constitutes a positive nipple margin. While a positive margin is most commonly understood as any tumor within the separate nipple margin, it leaves room for interpretation. We evaluated the way in which a positive nipple margin was defined, treated, and the resulting oncologic outcomes in patients undergoing NSM at a large community-based hospital system.
Methods: A retrospective chart review was performed of all NSM in our hospital system from April 2010 to December 2021 in patients with a breast cancer diagnosis. Patient and tumor characteristics, treatment, and outcomes information were collected, and descriptive analysis performed.
Results: 619 patients were included, comprising 1086 NSM, 617 of which were therapeutic and 469 prophylactic. Invasive ductal cancer (IDC) and ductal carcinoma in situ (DCIS) accounted for 77.3% of diagnoses and 10.8% were invasive lobular. Median tumor size was 1.7cm (range 0-14cm) and median follow-up was 30 months (range 0-128 months). 14 therapeutic NSM and 0 prophylactic NSM had tumor within the separate nipple margin. 11 of 14 nipple margins containing tumor were classified as positive using the definition, “any tumor within the separate nipple margin,” and subsequently underwent nipple-areolar complex (NAC) excision. 2 nipple margins containing tumor were classified as negative when a positive nipple margin was defined more specifically as “any tumor on ink” and underwent observation. The average time to NAC excision was 5.3 weeks (range 2-22 weeks), including one with residual IDC in the NAC excised concurrently with expander to implant exchange at 22 weeks. Of the 11 excised NAC, 4 had residual disease, 3 with DCIS and 1 with IDC. Only 4 recurrences were observed in all 619 (0.65%) patients undergoing NSM. Specifically, no recurrences were observed in those patients with tumor in the nipple margin who did not undergo subsequent NAC excision.
Conclusion: Our results suggest that the definition of a positive nipple margin warranting NAC excision could be interpreted as “any tumor on ink,” with observation of nipple margins containing tumor but without tumor at an inked edge. Delayed excision of the NAC may also be considered to coincide with staged reconstruction. Overall, NSM can be safely performed with low rates of positive nipple margins in high-volume community hospitals with exceptionally low rates of recurrence at the preserved NAC or loco-regionally.
Methods: A retrospective chart review was performed of all NSM in our hospital system from April 2010 to December 2021 in patients with a breast cancer diagnosis. Patient and tumor characteristics, treatment, and outcomes information were collected, and descriptive analysis performed.
Results: 619 patients were included, comprising 1086 NSM, 617 of which were therapeutic and 469 prophylactic. Invasive ductal cancer (IDC) and ductal carcinoma in situ (DCIS) accounted for 77.3% of diagnoses and 10.8% were invasive lobular. Median tumor size was 1.7cm (range 0-14cm) and median follow-up was 30 months (range 0-128 months). 14 therapeutic NSM and 0 prophylactic NSM had tumor within the separate nipple margin. 11 of 14 nipple margins containing tumor were classified as positive using the definition, “any tumor within the separate nipple margin,” and subsequently underwent nipple-areolar complex (NAC) excision. 2 nipple margins containing tumor were classified as negative when a positive nipple margin was defined more specifically as “any tumor on ink” and underwent observation. The average time to NAC excision was 5.3 weeks (range 2-22 weeks), including one with residual IDC in the NAC excised concurrently with expander to implant exchange at 22 weeks. Of the 11 excised NAC, 4 had residual disease, 3 with DCIS and 1 with IDC. Only 4 recurrences were observed in all 619 (0.65%) patients undergoing NSM. Specifically, no recurrences were observed in those patients with tumor in the nipple margin who did not undergo subsequent NAC excision.
Conclusion: Our results suggest that the definition of a positive nipple margin warranting NAC excision could be interpreted as “any tumor on ink,” with observation of nipple margins containing tumor but without tumor at an inked edge. Delayed excision of the NAC may also be considered to coincide with staged reconstruction. Overall, NSM can be safely performed with low rates of positive nipple margins in high-volume community hospitals with exceptionally low rates of recurrence at the preserved NAC or loco-regionally.

