Back
Trauma
Category: Quickshot Oral Session 20
Quickshot Oral : Quickshot Oral Session 20
EVALUATION OF INTERN ACCURACY IN DETECTION OF PNEUMOTHORAX USING EFAST
Monday, February 13, 2023
7:00am – 8:00am East Coast USA Time
- SI
Stephen Iacono, MD
United States
- JT
Jennifer To, DO
Trauma Surgeon
St. Luke's University Health Network, United States
Presenter(s)
Principal Contact(s)
Objectives: Cavitary triage is crucial in initial management of trauma patients, where the presence of free fluid or pneumothorax (PTX) could warrant emergent procedural intervention. Advanced Trauma Life Support (ATLS) teaches that imaging, such as xrays and ultrasound, are useful adjuncts to quickly identify life-threatening injuries within the trauma bay. The accuracy of the Extended Focused Assessment with Sonography in Trauma (eFAST) has recently come under scrutiny. The current literature suggests that eFAST accuracy depends on the experience of the provider performing the exam. In our study, we evaluate intern level residents (PGY1) that are designated to perform an eFAST exam during the trauma assessment.
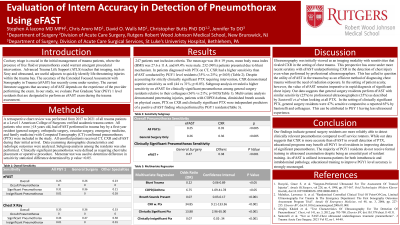
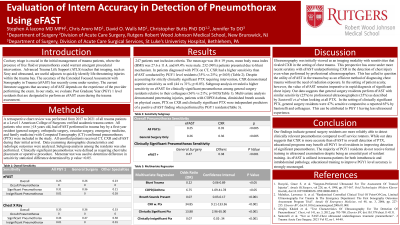
Methods: A retrospective review from 2017 to 2021 of all trauma patients at a Level 1 trauma center was performed. Patients who were ≥18 years old, had eFAST performed in trauma bay by a PGY1 resident (general surgery, orthopedic surgery, vascular surgery, emergency medicine, and family medicine) and diagnosed with PTX based on computed tomography (CT) were included. Exclusion criteria were patients without eFAST, CXR and CT scan. Demographic characteristics and radiologic outcomes were analyzed. Subgroup analysis among residents was performed.
Results: 247 patients met inclusion criteria. 96% (n=232) presented due to blunt mechanism. 69.4% were male, the mean age was 46 years, and the mean body mass index was 27.6 ± 11.4. In patients diagnosed with PTX on CT, CXR had a higher sensitivity than eFAST (35% vs 25%; p< 0.05). Despite accounting for strictly clinically significant PTX requiring intervention, CXR demonstrated superior sensitivity as well (44 vs 31%; p< 0.05). Subgroup analysis revealed a higher sensitivity on eFAST for clinically significant PTX among general surgery residents relative to their colleagues (36% vs 21%; p< 0.05). Multivariate analysis demonstrated penetrating injuries, patients with COPD/Asthma, diminished breath sounds on physical exam, PTX on CXR and clinically significant PTX are predictors of a positive eFAST finding when performed by PGY1 residents.
Conclusion: Our study shows that PGY1 residents peforming eFAST were less sensitive than CXR for diagnosing PTX. Although general surgery residents had higher sensitivity than off service residents in diagnosing clinically significant PTX, our study shows CXR to be superior to eFAST in overall detection of PTX in early trainees. Ultrasound based educational programs may benefit PGY1 level residents in improving eFAST detection of intrathoracic pathology. As eFAST is utilized in trauma patients for both intrathoracic and intrabdominal pathology, educational training to improve resident accuracy is strongly encouraged.
Methods: A retrospective review from 2017 to 2021 of all trauma patients at a Level 1 trauma center was performed. Patients who were ≥18 years old, had eFAST performed in trauma bay by a PGY1 resident (general surgery, orthopedic surgery, vascular surgery, emergency medicine, and family medicine) and diagnosed with PTX based on computed tomography (CT) were included. Exclusion criteria were patients without eFAST, CXR and CT scan. Demographic characteristics and radiologic outcomes were analyzed. Subgroup analysis among residents was performed.
Results: 247 patients met inclusion criteria. 96% (n=232) presented due to blunt mechanism. 69.4% were male, the mean age was 46 years, and the mean body mass index was 27.6 ± 11.4. In patients diagnosed with PTX on CT, CXR had a higher sensitivity than eFAST (35% vs 25%; p< 0.05). Despite accounting for strictly clinically significant PTX requiring intervention, CXR demonstrated superior sensitivity as well (44 vs 31%; p< 0.05). Subgroup analysis revealed a higher sensitivity on eFAST for clinically significant PTX among general surgery residents relative to their colleagues (36% vs 21%; p< 0.05). Multivariate analysis demonstrated penetrating injuries, patients with COPD/Asthma, diminished breath sounds on physical exam, PTX on CXR and clinically significant PTX are predictors of a positive eFAST finding when performed by PGY1 residents.
Conclusion: Our study shows that PGY1 residents peforming eFAST were less sensitive than CXR for diagnosing PTX. Although general surgery residents had higher sensitivity than off service residents in diagnosing clinically significant PTX, our study shows CXR to be superior to eFAST in overall detection of PTX in early trainees. Ultrasound based educational programs may benefit PGY1 level residents in improving eFAST detection of intrathoracic pathology. As eFAST is utilized in trauma patients for both intrathoracic and intrabdominal pathology, educational training to improve resident accuracy is strongly encouraged.

