Back
Vascular
Category: Quickshot Oral Session 17
Quickshot Oral : Quickshot Oral Session 17
COLLATERAL DAMAGE: THE IMPORTANCE OF THE HYPOGASTRIC AND PROFUNDA FEMORIS ARTERY
Monday, February 13, 2023
7:00am – 8:00am East Coast USA Time

Gabrielle Moore, MD
General Surgery Resident
Medical College of Georgia, United States- MS
Mrinal Shukla, MD
United States
Presenter(s)
Principal Contact(s)
Objectives:
Introduction:
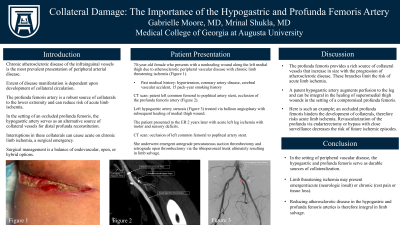
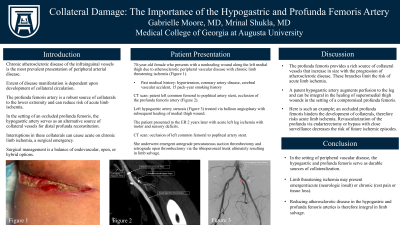
Atherosclerotic peripheral vascular disease management is performed with a balance of endovascular, open, and hybrid options. Varying presentations are based on the extensive collateral circulation that develops based on demand and activity. Lower extremity circulation, specifically thigh, relies on the iliofemoral arteries. In the setting of occlusive disease, the profunda femoris is a good source of perfusion can reduce risk of acute limb ischemia. However, in the setting of an occluded profunda, the hypogastric artery serves to increase perfusion to collateral vessels for distal profunda reconstitution. Interruptions in these collaterals can cause acute on chronic limb ischemia, a surgical emergency.
Case Presentation:
A 70 year old female presents with a nonhealing wound along the medial thigh despite multiple debridements by the general surgery team. A computed tomography scan with contrast of the leg showed stents from the common femoral artery to the popliteal artery with an occluded profunda femoris artery in addition to an ipsilateral hypogastric artery stenosis. She underwent balloon angioplasty of the hypogastric artery with subsequent healing of medial thigh wound. Ten months later, the patient returned with acute limb ischemia and occluded infrainguinal stents with subsequent thrombosis of the external iliac, common femoral, superficial femoral and popliteal artery manifesting as motor deficits. We proceeded to the operating room emergently for an antegrade percutaneous suction thrombectomy and retrograde open thrombectomy via the tibioperoneal trunk resulting in limb salvage.
Discussion:
The profunda femoris is a rich source of collateral vessels that increase in size with the progression of atherosclerotic disease in the superficial femoral artery. Its branches reconstitute the distal SFA or popliteal artery via genicular arteries. These branches therefore perfuse the leg and limit risk of limb loss in an acute or chronic basis. Additionally, a healthy hypogastric artery augments perfusion to the leg and can be integral in the healing of a medial thigh or upper thigh wound. We present such a case however, an occluded profunda hinders the development of collaterals and therefore risks acute limb ischemia. Revascularization of the profunda via endarterectomy or bypass and close surveillance will help decrease the risk of future ischemic episodes.
Conclusion:
Our patient displays the consequences of an occluded profunda femoris artery and the important network of collaterals that derive from it along with the hypogastric artery. A nonhealing wound or acute limb ischemia can be limb threatening and require an above knee amputation without revascularization.
Methods:
Results:
Conclusion:
Introduction:
Atherosclerotic peripheral vascular disease management is performed with a balance of endovascular, open, and hybrid options. Varying presentations are based on the extensive collateral circulation that develops based on demand and activity. Lower extremity circulation, specifically thigh, relies on the iliofemoral arteries. In the setting of occlusive disease, the profunda femoris is a good source of perfusion can reduce risk of acute limb ischemia. However, in the setting of an occluded profunda, the hypogastric artery serves to increase perfusion to collateral vessels for distal profunda reconstitution. Interruptions in these collaterals can cause acute on chronic limb ischemia, a surgical emergency.
Case Presentation:
A 70 year old female presents with a nonhealing wound along the medial thigh despite multiple debridements by the general surgery team. A computed tomography scan with contrast of the leg showed stents from the common femoral artery to the popliteal artery with an occluded profunda femoris artery in addition to an ipsilateral hypogastric artery stenosis. She underwent balloon angioplasty of the hypogastric artery with subsequent healing of medial thigh wound. Ten months later, the patient returned with acute limb ischemia and occluded infrainguinal stents with subsequent thrombosis of the external iliac, common femoral, superficial femoral and popliteal artery manifesting as motor deficits. We proceeded to the operating room emergently for an antegrade percutaneous suction thrombectomy and retrograde open thrombectomy via the tibioperoneal trunk resulting in limb salvage.
Discussion:
The profunda femoris is a rich source of collateral vessels that increase in size with the progression of atherosclerotic disease in the superficial femoral artery. Its branches reconstitute the distal SFA or popliteal artery via genicular arteries. These branches therefore perfuse the leg and limit risk of limb loss in an acute or chronic basis. Additionally, a healthy hypogastric artery augments perfusion to the leg and can be integral in the healing of a medial thigh or upper thigh wound. We present such a case however, an occluded profunda hinders the development of collaterals and therefore risks acute limb ischemia. Revascularization of the profunda via endarterectomy or bypass and close surveillance will help decrease the risk of future ischemic episodes.
Conclusion:
Our patient displays the consequences of an occluded profunda femoris artery and the important network of collaterals that derive from it along with the hypogastric artery. A nonhealing wound or acute limb ischemia can be limb threatening and require an above knee amputation without revascularization.
Methods:
Results:
Conclusion:

