Colorectal
Category: Quickshot Oral Session 03
Quickshot Oral : Quickshot Oral Session 03
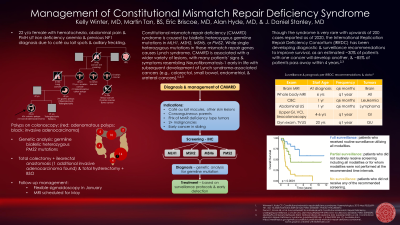
MANAGEMENT OF CONSTITUTIONAL MISMATCH REPAIR DEFICIENCY SYNDROME
Saturday, February 11, 2023
3:00pm - 4:00pm East Coast USA Time
- MT
Martin Tan, BS
Medical Student
University of Tennessee Health Science Center - KW
Kelly Winter, MD
United States
Presenter(s)
Principal Contact(s)
Objectives: Patient is a 22 year old female who presented with occasional painless rectal bleeding and underwent colonoscopy; she was found to have greater than forty polyps that were removed. Pathology of these polyps revealed primarily tubular adenomas with one sigmoid biopsy showing invasive adenocarcinoma with loss of expression of MSH6 and PMS2. The patient’s medical history includes a clinical diagnosis of neurofibromatosis type 1 based on cafe au lait spots and Lisch nodules. She underwent total thyroidectomy at age seventeen for a symptomatic thyroid nodule that returned benign nontoxic goiter. Her family history includes that both parents are adopted: father with unknown family history. Her maternal grandmother had a history of ovarian cancer and precancerous polyps. Multiple others in the maternal pedigree had ovarian and breast cancer. The patient’s brother, age 21, has epilepsy. Her young age and loss of expression of MSH6/PMS2 by IHC prompted genetic testing, which revealed two separate pathogenic mutations on the PMS2 gene, making her heterozygous for each of these. They are suspected to be on different chromosomes (in trans), thus causing Constitutional Mismatch Repair Deficiency (CMMRD). PMS2 mutations confer an increased risk of colon (15-20% lifetime) and endometrial (15% lifetime) cancer, as well as other cancers. CMMRD syndrome is a rare autosomal recessive disorder characterized by cafe au lait macules as well as increased risk of hematologic malignancies, brain tumors, and early onset Lynch syndrome-associated cancers. Nearly all patients have cafe au lait macules, and presumably, our patient does not have neurofibromatosis, but rather CMMRD. Current considerations for our patient include a total colectomy and a prophylactic hysterectomy and oophorectomy. Ongoing surveillance and vigilant screening will be required for her as well as her family members, and genetic testing is recommended for her family members. The International Replication Repair Deficiency Consortium (IRRDC) is composed of clinicians and scientists from more than 45 countries and provides guidance for patients and providers. The IRRDC surveillance protocol has allowed for all GI and solid tumors and 75% of brain tumors to be detected asymptomatically, with a 90% 5-year-survival for patients with cancers detected asymptomatically. Current recommendations for colon cancer treatment are similar to sporadic colon cancers with the addition of PET imaging for any diagnosed cancer, although individualized treatment should be considered with respect to polyp burden, prevalence of extracolonic tumors, and overall prognosis.
Methods:
Results:
Conclusion:
Methods:
Results:
Conclusion:

