Back
GI
Category: Quickshot Oral Session 21
Quickshot Oral : Quickshot Oral Session 21
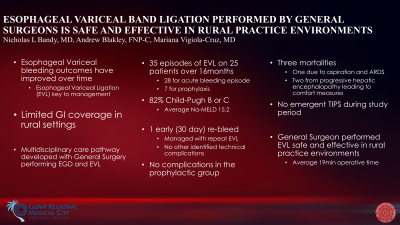
ESOPHAGEAL VARICEAL BAND LIGATION PERFORMED BY GENERAL SURGEONS IS SAFE AND EFFECTIVE IN RURAL PRACTICE ENVIRONMENTS
Monday, February 13, 2023
7:00am – 8:00am East Coast USA Time
Nicholas Bandy, MD
Surgeon
Guam Regional Medical City, United States
Nicholas Bandy, MD
Surgeon
Guam Regional Medical City, United States
Presenter(s)
Principal Contact(s)
Objectives: Acute hemorrhage occurs in up to one third of cirrhotic patients with esophageal varices, often presenting as a life-threatening bleed. Standard management includes resuscitation, prompt medical treatment, and urgent endoscopy with variceal band ligation (VBL) or sclerotherapy. Gastroenterology services are not always available in rural hospitals. A multidisciplinary gastrointestinal bleed protocol was initiated at our institution, with on call Emergency General Surgeons performing upper endoscopy for all suspected variceal hemorrhage with VBL if indicated. VBL was also introduced in our institution for both primary and secondary prophylaxis against variceal hemorrhage.
Methods: All patients who underwent VBL at our institution during the 16 month study period were included for review. Indication for endoscopy and the etiology and severity of cirrhosis were obtained. Outcomes including treatment failure (thirty day re-bleed), procedural complications, readmission and mortality were recorded.
Results: Following initiation of the variceal bleed protocol, 25 patients underwent VBL a total of 35 times. The procedure was performed for acute bleeding 28 times, and as prophylaxis 7 times. In the acutely bleeding population, we observed an average Na-MELD of 15.25 with 82% of patients having a Child-Pugh score of B or C. We recorded no technical complications from the endoscopic band ligation procedure. There was one episode of early rebleeding following intervention for acute hemorrhage (3.5%), two readmissions within 30 days (7.1%) and three mortalities within 30 days (10.7%). None of the prophylactic procedures had a post operative complication, bleeding event, or mortality; there was one admission within 30 days for an unrelated medical event following prophylactic VBL.
Conclusion: VBL performed by General Surgeons in rural practice environments has an acceptable safety profile with high rates of technical success.
Methods: All patients who underwent VBL at our institution during the 16 month study period were included for review. Indication for endoscopy and the etiology and severity of cirrhosis were obtained. Outcomes including treatment failure (thirty day re-bleed), procedural complications, readmission and mortality were recorded.
Results: Following initiation of the variceal bleed protocol, 25 patients underwent VBL a total of 35 times. The procedure was performed for acute bleeding 28 times, and as prophylaxis 7 times. In the acutely bleeding population, we observed an average Na-MELD of 15.25 with 82% of patients having a Child-Pugh score of B or C. We recorded no technical complications from the endoscopic band ligation procedure. There was one episode of early rebleeding following intervention for acute hemorrhage (3.5%), two readmissions within 30 days (7.1%) and three mortalities within 30 days (10.7%). None of the prophylactic procedures had a post operative complication, bleeding event, or mortality; there was one admission within 30 days for an unrelated medical event following prophylactic VBL.
Conclusion: VBL performed by General Surgeons in rural practice environments has an acceptable safety profile with high rates of technical success.

