Pediatrics
Category: Quickshot Oral Session 14
Quickshot Oral : Quickshot Oral Session 14
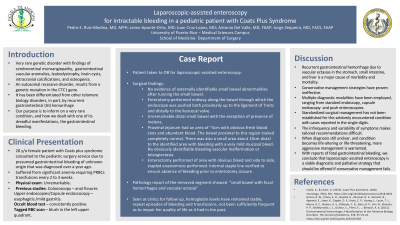
LAPAROSCOPIC-ASSISTED ENTEROSCOPY FOR INTRACTABLE BLEEDING IN A PEDIATRIC PATIENT WITH COATS PLUS SYNDROME
Sunday, February 12, 2023
7:00am - 8:00am East Coast USA Time
- PR
Pedro E. Ruiz-Medina, MD, MPH
Resident
University of Puerto Rico, United States - PR
Pedro E. Ruiz-Medina, MD, MPH
Resident
University of Puerto Rico, United States
Presenter(s)
Principal Contact(s)
Objectives: Coats plus syndrome (CP) is a rare genetic disorder associated to premature telomere shortening leading to a multi-systemic disease which include primarily cerebroretinal microangiopathy as well as gastrointestinal vascular anomalies, leukodystrophy, brain cysts, intracranial calcifications, and osteopenia. The purpose of this report is to shed light on a very rare condition, and how we dealt with one of its dreadful manifestations, the gastrointestinal bleeding.
This is the case of a 20 y/o female patient with CP syndrome, that was consulted to the pediatric surgery service due to presumed gastrointestinal bleeding of unknown origin. She has had this complication since over a year ago. Endoscopic studies had revealed esophagitis and mild gastritis. The patient continued with significant anemia and had been requiring PRBCs transfusions every 2 to 3 weeks. A tagged RBC scan showed a blush in the left upper quadrant. The patient was taken to the OR for a laparoscopic-assisted enteroscopy where an area of bleeding was found in the proximal jejunum. Segmental enterectomy was performed with anastomosis and she was discharged home a few days later without complications. The pathology report showed “focal hemorrhages and vascular ectasia”. The patient was seen at clinics for follow up, hemoglobin levels have remained stable, and even though there have been repeat episodes of bleeding and transfusions, these have not been sufficiently frequent as to impair her quality of life as it had in the past.
CP is characterized, in part, by recurrent gastrointestinal hemorrhage due to vascular ectasias in the stomach, small intestine, and liver. This is a major cause of morbidity, and traditionally, conservative management strategies have proven ineffective. In the search for answers, multiple diagnostic modalities have been employed, ranging from standard endoscopy, capsule endoscopy and push enteroscopies. Our case shows that when the diagnosis is still unclear, and the condition becomes life-altering or life-threatening, more aggressive management is warranted.
Standardized surgical management has not been established for this seldomly encountered condition with cases reported in the single digits. The infrequency and variability of symptoms makes tailored recommendations difficult. With reports of fatal gastrointestinal bleeding, we conclude that laparoscopic-assisted enteroscopy is a viable diagnostic and palliative strategy that should be offered if conservative management fails.
Methods:
Results:
Conclusion:
This is the case of a 20 y/o female patient with CP syndrome, that was consulted to the pediatric surgery service due to presumed gastrointestinal bleeding of unknown origin. She has had this complication since over a year ago. Endoscopic studies had revealed esophagitis and mild gastritis. The patient continued with significant anemia and had been requiring PRBCs transfusions every 2 to 3 weeks. A tagged RBC scan showed a blush in the left upper quadrant. The patient was taken to the OR for a laparoscopic-assisted enteroscopy where an area of bleeding was found in the proximal jejunum. Segmental enterectomy was performed with anastomosis and she was discharged home a few days later without complications. The pathology report showed “focal hemorrhages and vascular ectasia”. The patient was seen at clinics for follow up, hemoglobin levels have remained stable, and even though there have been repeat episodes of bleeding and transfusions, these have not been sufficiently frequent as to impair her quality of life as it had in the past.
CP is characterized, in part, by recurrent gastrointestinal hemorrhage due to vascular ectasias in the stomach, small intestine, and liver. This is a major cause of morbidity, and traditionally, conservative management strategies have proven ineffective. In the search for answers, multiple diagnostic modalities have been employed, ranging from standard endoscopy, capsule endoscopy and push enteroscopies. Our case shows that when the diagnosis is still unclear, and the condition becomes life-altering or life-threatening, more aggressive management is warranted.
Standardized surgical management has not been established for this seldomly encountered condition with cases reported in the single digits. The infrequency and variability of symptoms makes tailored recommendations difficult. With reports of fatal gastrointestinal bleeding, we conclude that laparoscopic-assisted enteroscopy is a viable diagnostic and palliative strategy that should be offered if conservative management fails.
Methods:
Results:
Conclusion:

