Back
Pediatrics
Category: Quickshot Oral Session 26
Quickshot Oral : Quickshot Oral Session 26
ERCP FINDINGS PROVIDE FURTHER JUSTIFICATION FOR A SURGERY FIRST MINDSET IN PEDIATRIC CHOLEDOCHOLITHIASIS
Tuesday, February 14, 2023
7:00am – 8:00am East Coast USA Time

Gloria Sanin, MD
Surgical Resident
Wake Forest University School of Medicine, United States- AP
Allison Perko, BS
United States
Presenter(s)
Principal Contact(s)
Objectives: Endoscopic retrograde cholangiopancreatography (ERCP) first pathway is heavily favored in the management of choledocholithiasis for pediatric patients, despite often requiring two separate general anesthetics. In contrast, a single-stage, “surgery first”, an approach consisting of LC with cholangiogram and possible laparoscopic common bile duct exploration (LCBDE), has a shorter length of stay with an equivalent safety profile. However, it is unclear what proportion of pediatric patients undergoing initial ERCP have endoscopic evidence of obstructions that would be amenable to clearance with LCBDE. We hypothesized the majority of patients who obtained an ERCP before LC would have been candidates for and benefited from initial LCBDE for choledocholithiasis during LC.
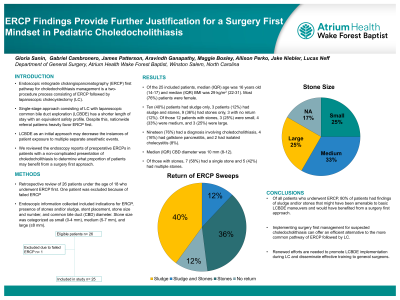
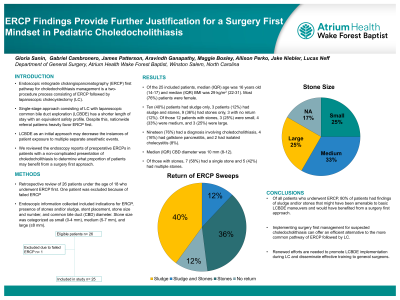
Methods: A retrospective review of all patients under the age of 18 at a single children’s hospital who underwent ERCP before LC over a 10 year period was conducted. Twenty-six patients underwent ERCP before LC, with 1 patient excluded due to a failed ERCP attempt. Demographic and endoscopic data were analyzed, including ERCP indications, presence of stones or sludge, stone size and number, and stent placement. Based on accepted criteria, stone size was categorized as small (0-4 mm), medium (5-7 mm), or large (≥8 mm). Findings considered amenable to LCBDE included the presence of no return, sludge, or stones less than 8 mm on ERCP.
Results: Of the twenty-five ERCPs analyzed, 10 (40%) had sludge only, 3 (12%) had sludge and stones removed, 9 (36%) had only stones removed, and 3 (12%) had no evidence of stones or sludge. In the 12 patients with stones removed, 3 (25%) had small stones, 4 (33%) had medium stones, and 3 (25%) had large stones; stone size was not specified in 2 patients. Twelve patients had choledocholithiasis with cholelithiasis (48%), making it the most common primary indication for ERCP, followed by primary choledocholithiasis (24%), gallstone pancreatitis (16%), cholecystitis (8%), and concomitant choledocholithiasis with cholecystitis (4%). Of all patients who underwent ERCP, 80% had either findings of sludge, stones amenable to LCBDE maneuvers, or no return of material after balloon sweeps.
Conclusion: Our findings suggest that a large majority (80%) of pediatric patients who underwent preoperative ERCP had obstructions that are amenable to LCBDE. Implementing surgery first management for suspected choledocholithiasis can offer an efficient pathway to the more established ERCP first strategy. Renewed efforts are needed to promote LCBDE implementation during LC and disseminate practical training to pediatric surgeons.
Methods: A retrospective review of all patients under the age of 18 at a single children’s hospital who underwent ERCP before LC over a 10 year period was conducted. Twenty-six patients underwent ERCP before LC, with 1 patient excluded due to a failed ERCP attempt. Demographic and endoscopic data were analyzed, including ERCP indications, presence of stones or sludge, stone size and number, and stent placement. Based on accepted criteria, stone size was categorized as small (0-4 mm), medium (5-7 mm), or large (≥8 mm). Findings considered amenable to LCBDE included the presence of no return, sludge, or stones less than 8 mm on ERCP.
Results: Of the twenty-five ERCPs analyzed, 10 (40%) had sludge only, 3 (12%) had sludge and stones removed, 9 (36%) had only stones removed, and 3 (12%) had no evidence of stones or sludge. In the 12 patients with stones removed, 3 (25%) had small stones, 4 (33%) had medium stones, and 3 (25%) had large stones; stone size was not specified in 2 patients. Twelve patients had choledocholithiasis with cholelithiasis (48%), making it the most common primary indication for ERCP, followed by primary choledocholithiasis (24%), gallstone pancreatitis (16%), cholecystitis (8%), and concomitant choledocholithiasis with cholecystitis (4%). Of all patients who underwent ERCP, 80% had either findings of sludge, stones amenable to LCBDE maneuvers, or no return of material after balloon sweeps.
Conclusion: Our findings suggest that a large majority (80%) of pediatric patients who underwent preoperative ERCP had obstructions that are amenable to LCBDE. Implementing surgery first management for suspected choledocholithiasis can offer an efficient pathway to the more established ERCP first strategy. Renewed efforts are needed to promote LCBDE implementation during LC and disseminate practical training to pediatric surgeons.

