Back
Cancer
Category: Quickshot Oral Session 02
Quickshot Oral : Quickshot Oral Session 02
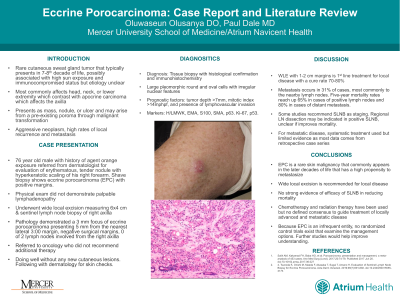
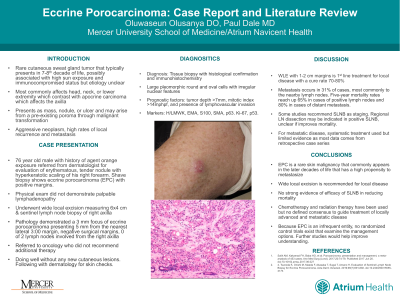
ECCRINE POROCARCINOMA: A CASE PRESENTATION AND REVIEW OF THE LITERATURE
Saturday, February 11, 2023
3:00pm – 4:00pm East Coast USA Time

Oluwaseun Olusanya, DO
Surgical Resident
Atrium Health Navicent, United States- pD
paul S. Dale, MD
Atrium Health Navicent, United States
Presenter(s)
Principal Contact(s)
Objectives: Eccrine porocarcinoma (EPC) is a rare adnexal skin cancer arising from the eccrine sweat glands. Due to the rarity of the cancer, there are no guidelines for management. A 76-year-old male presents with a right forearm lesion that had been present for over 20 years. Shave biopsies demonstrated eccrine porocarcinoma. Physical examination showed a 1cm erythematous, hyperkeratotic nodule. CT scans were negative for any metastatic lesions. Patient underwent wide local excision and sentinel lymph node biopsy (SLNB). Pathology demonstrated 3mm focus of EPC with negative margins and no involved lymph nodes in the right axilla. He was referred to oncology who did not recommend any additional therapy. EPC is an aggressive neoplasm with a high rate of local recurrence and metastasis often present at time of diagnosis. It typically presents in the 7th decade of life and most commonly affects the head and neck, followed by the lower extremity. Due to its variable presentation, it has a very broad differential. As a result, tissue biopsy with histological confirmation is necessary for diagnosis. EPC typically demonstrates large pleomorphic round cells with an irregular nucleus and prominent nucleoli arranged in lobules infiltrating the dermal tissue of the sweat gland. Histological characteristics that have prognostic importance include a tumor depth >7mm, >4 mitoses per hpf, and the presence of lymphovascular invasion. Though there is no single marker for EPC, EMA, SMA, and S100 can help differentiate cells of eccrine origin. Surgery is the mainstay of therapy for local disease with wide local excision with 1-2cm margins having a cure rate of 70-80%. Unfortunately, 31% of cases have metastasis to lymph nodes on presentation. These patients have a 5-year mortality rate of up to 65%. As result, evaluation of regional lymph nodes in clinically node negative patients with SLNB has become more prominent. However, it has not been demonstrated if SLNB improves the mortality rate in this patient group. Some studies have shown promising results with adjuvant radiation in local disease with high-risk histological features, tumors size >5 cm, and positive surgical margins. For metastatic or inoperable disease, systemic treatments have been employed with varying results however there is limited evidence supporting their efficacy as existing data is based on retrospective case series. There remains no treatment protocol or standardized chemotherapeutic regimen. Multi-institutional collaboration would be necessary to recruit sufficient patients to develop therapies and guidelines to treat those diagnosed with EPC.
Methods:
Results:
Conclusion:
Methods:
Results:
Conclusion:

