General Surgery
Category: Quickshot Oral Session 04
Quickshot Oral : Quickshot Oral Session 04
SMOKING IS THE CULPRIT - UMBILICAL HERNIA RATE AFTER LAPAROSCOPIC AND LAPAROENDOSCOPIC SINGLE-SITE CHOLECYSTECTOMY
Saturday, February 11, 2023
3:00pm - 4:00pm East Coast USA Time
.jpg)
Emily Sardzinski
Research Assistant
Florida Surgical Specialists, United States- PT
Paul Toomey, MD
United States
Presenter(s)
Principal Contact(s)
Objectives: A multiport laparoscopic cholecystectomy is the current standard operation for the management of benign gallbladder diseases. Laparoendoscopic Single-Site (LESS) cholecystectomy offers improved cosmesis through a single umbilical incision. The aim of this study was to analyze umbilical hernia occurrences in patients who underwent laparoscopic or LESS cholecystectomy.
Methods: Patients who underwent laparoscopic or LESS cholecystectomy undertaken by a single surgeon between 2015 to 2020 were surveyed with a questionnaire by phone call or email. Data are presented as median (mean +/- standard deviation).
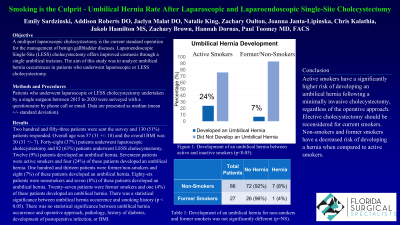
Results: Two hundred and fifty-three patients were sent the survey and 130 (51%) patients responded. The overall age was 57 (31 +/- 18) and the overall BMI was 30 (31 +/- 7). Forty-eight (37%) patients underwent laparoscopic cholecystectomy and 82 (63%) patients underwent LESS cholecystectomy. Twelve (9%) patients developed an umbilical hernia. Seventeen patients were active smokers and four (24%) of these patients developed an umbilical hernia. One hundred and thirteen patients were not active smokers and eight (7%) of these patients developed an umbilical hernia. Eighty-six patients were nonsmokers and seven (8%) of these patients developed an umbilical hernia. Twenty-seven patients were former smokers and one (4%) of these patients developed an umbilical hernia. There was a statistical significance between umbilical hernia occurrence and smoking history (p < 0.05). There was no statistical significance between umbilical hernia occurrence and operative approach, pathology, history of diabetes, development of postoperative infection, or BMI (p = ns).
Conclusion: Active smokers have a significantly higher risk of developing an umbilical hernia following a minimally invasive cholecystectomy, regardless of the operative approach. Elective cholecystectomy should be reconsidered for current smokers. Nonsmokers or former smokers have a decreased risk of developing a hernia when compared to active smokers.
Methods: Patients who underwent laparoscopic or LESS cholecystectomy undertaken by a single surgeon between 2015 to 2020 were surveyed with a questionnaire by phone call or email. Data are presented as median (mean +/- standard deviation).
Results: Two hundred and fifty-three patients were sent the survey and 130 (51%) patients responded. The overall age was 57 (31 +/- 18) and the overall BMI was 30 (31 +/- 7). Forty-eight (37%) patients underwent laparoscopic cholecystectomy and 82 (63%) patients underwent LESS cholecystectomy. Twelve (9%) patients developed an umbilical hernia. Seventeen patients were active smokers and four (24%) of these patients developed an umbilical hernia. One hundred and thirteen patients were not active smokers and eight (7%) of these patients developed an umbilical hernia. Eighty-six patients were nonsmokers and seven (8%) of these patients developed an umbilical hernia. Twenty-seven patients were former smokers and one (4%) of these patients developed an umbilical hernia. There was a statistical significance between umbilical hernia occurrence and smoking history (p < 0.05). There was no statistical significance between umbilical hernia occurrence and operative approach, pathology, history of diabetes, development of postoperative infection, or BMI (p = ns).
Conclusion: Active smokers have a significantly higher risk of developing an umbilical hernia following a minimally invasive cholecystectomy, regardless of the operative approach. Elective cholecystectomy should be reconsidered for current smokers. Nonsmokers or former smokers have a decreased risk of developing a hernia when compared to active smokers.

