Back
Vascular
Category: Quickshot Oral Session 17
Quickshot Oral : Quickshot Oral Session 17
ENDOVASCULAR MANAGEMENT OF A SYMPTOMATIC GIANT HEPATIC ARTERY ANEURYSM
Monday, February 13, 2023
7:00am – 8:00am East Coast USA Time
- AC
Anthony Clark, MD
Surgical Resident
University of Louisville, United States - AC
Anthony Clark, MD
Surgical Resident
University of Louisville, United States
Presenter(s)
Principal Contact(s)
Objectives: Hepatic artery aneurysms (HAA) are an uncommon clinical condition. Ruptured hepatic artery aneurysms carry a high incidence of mortality. Traditionally, they are treated with open surgical resection; however, endovascular aneurysm exclusion is an alternative option to open repair in select patients who have suitable anatomy.
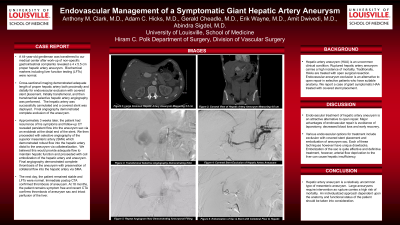
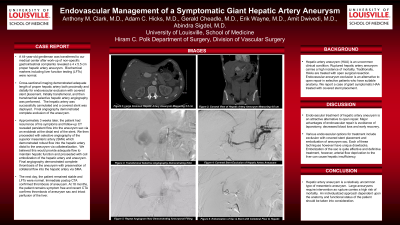
A 44-year-old gentleman was transferred to our medical center after work-up for right upper quadrant pain revealed a 4 x 5.5 cm proper hepatic artery aneurysm. Biochemical markers including liver function testing were normal. Cross-sectional imaging demonstrated adequate length of proper hepatic artery both proximally and distally for endovascular exclusion with covered stent placement. Initially, transfemoral followed by transbrachial selective hepatic artery angiography was performed. The hepatic artery was successfully cannulated, and a covered stent was deployed. Final angiography demonstrated complete exclusion of the aneurysm. The patient’s pain was relieved; however, 3 weeks later, the patient re-presented with right upper quadrant pain. CT revealed persistent flow into the aneurysm sac via a leak at the distal end of the stent. We elected to proceed with selective angiography of the superior mesenteric artery (SMA), which demonstrated robust flow into the hepatic artery distal to the aneurysm via collateralization. We believed this would provide adequate flow to maintain hepatic function and proceeded with coil embolization of the hepatic artery and aneurysm as there was no room for distal stent placement. Final angiography demonstrated complete thrombosis of the aneurysm with preservation of collateral flow into the hepatic artery via the SMA. Postoperatively, the patient’s pain was resolved. Immediate postoperative CTA confirmed thrombosis of the aneurysm. At 18 months, the patient remains symptom free and recent CTA confirms thrombosis of the aneurysm sac and intact perfusion of the liver.
Endovascular treatment of HAAs is an attractive alternative to open repair. Major advantages of endovascular repair are avoidance of laparotomy, decreased blood loss, and early recovery. Various endovascular options for treatment include exclusion with covered stent placement and embolization of the aneurysm sac. Each of these techniques, however, have unique drawbacks. Embolization of the sac is an effective and definitive treatment but risks causing hepatic insufficiency. In our case, robust collateralization from the SMA preserved hepatic flow.
Hepatic artery aneurysms are uncommon types of mesenteric aneurysms. Large aneurysms require intervention as rupture carries a high risk of mortality. An individualized approach dependent upon the anatomy and functional status of the patient should be taken into consideration.
Methods:
Results:
Conclusion:
A 44-year-old gentleman was transferred to our medical center after work-up for right upper quadrant pain revealed a 4 x 5.5 cm proper hepatic artery aneurysm. Biochemical markers including liver function testing were normal. Cross-sectional imaging demonstrated adequate length of proper hepatic artery both proximally and distally for endovascular exclusion with covered stent placement. Initially, transfemoral followed by transbrachial selective hepatic artery angiography was performed. The hepatic artery was successfully cannulated, and a covered stent was deployed. Final angiography demonstrated complete exclusion of the aneurysm. The patient’s pain was relieved; however, 3 weeks later, the patient re-presented with right upper quadrant pain. CT revealed persistent flow into the aneurysm sac via a leak at the distal end of the stent. We elected to proceed with selective angiography of the superior mesenteric artery (SMA), which demonstrated robust flow into the hepatic artery distal to the aneurysm via collateralization. We believed this would provide adequate flow to maintain hepatic function and proceeded with coil embolization of the hepatic artery and aneurysm as there was no room for distal stent placement. Final angiography demonstrated complete thrombosis of the aneurysm with preservation of collateral flow into the hepatic artery via the SMA. Postoperatively, the patient’s pain was resolved. Immediate postoperative CTA confirmed thrombosis of the aneurysm. At 18 months, the patient remains symptom free and recent CTA confirms thrombosis of the aneurysm sac and intact perfusion of the liver.
Endovascular treatment of HAAs is an attractive alternative to open repair. Major advantages of endovascular repair are avoidance of laparotomy, decreased blood loss, and early recovery. Various endovascular options for treatment include exclusion with covered stent placement and embolization of the aneurysm sac. Each of these techniques, however, have unique drawbacks. Embolization of the sac is an effective and definitive treatment but risks causing hepatic insufficiency. In our case, robust collateralization from the SMA preserved hepatic flow.
Hepatic artery aneurysms are uncommon types of mesenteric aneurysms. Large aneurysms require intervention as rupture carries a high risk of mortality. An individualized approach dependent upon the anatomy and functional status of the patient should be taken into consideration.
Methods:
Results:
Conclusion:

