General Surgery
Category: Quickshot Oral Session 04
Quickshot Oral : Quickshot Oral Session 04
SPLENIC RUPTURE AS AN INITIAL PRESENTATION OF DIFFUSE LARGE B-CELL LYMPHOMA
Saturday, February 11, 2023
3:00pm - 4:00pm East Coast USA Time
- JH
Joseph Hlopak, DO
General Surgery Resident
Crozer Health, Delaware, United States - PS
Praveen Satarasinghe, MD, MBA
United States
Presenter(s)
Principal Contact(s)
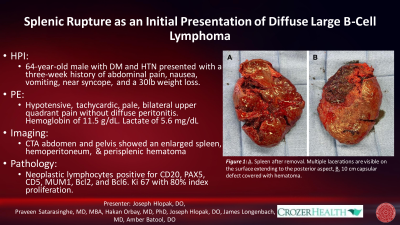
Objectives: Patient is a 64-year-old Caucasian male, history of diabetes mellitus type II, hypertension, and no prior history of trauma, who presented to the emergency department with a three-week history of abdominal pain, nausea, vomiting, and dizziness in the setting of 30-pound weight loss. On physical examination, he was hypotensive, tachycardic, and pale with tenderness in the right and left upper quadrants but no peritonitis. Fluid resuscitation resulted in temporary improvement of blood pressure with his initial laboratory results showing a hemoglobin of 11.5 g/dl and a lactate of 5.6 mg/dl. A computed tomography angiography (CTA) of the abdomen and pelvis illustrated hemoperitoneum and an enlarged spleen measuring 16.7 cm with an 8 mm arterial enhancing focus in the upper pole suspicious for pseudoaneurysm and perisplenic hematoma. Due to hemodynamic instability, the patient was taken to the operating room for an exploratory laparotomy and the spleen was found to be enlarged with a weight of 686 grams and dimensions of 18.5 x 14 x 5.5 cm. The capsule was heavily disrupted with a 10 cm defect opposite to the hilum filled with hematoma. The hilar aspect contained multiple 3-10 cm lacerations occupying approximately 50% of the surface area. Pathological exam of the spleen revealed soft pink-red spongy cut surface remarkable for diffuse intraparenchymal hematomas throughout. Neoplastic lymphocytes were positive for CD20, PAX5, CD5, MUM1, Bcl2, and Bcl6. Ki 67 staining showed a high proliferation index (80%) representing de Novo large B cell lymphoma or a transformation from a small lymphocytic lymphoma (B-CLL/SLL).
Non-traumatic splenic rupture is a rare initial presentation of hematological malignancies. In this case, we present a patient with undiagnosed diffuse large B cell lymphoma who presented to the emergency department with a delayed manifestation of splenic rupture and hemorrhagic shock requiring emergency splenectomy. High level of suspicion and simple bedside imaging methods can be highly sensitive in the diagnosis of non-traumatic splenic rupture. Timely intervention prevents mortality. In a stable patient, splenic salvage may be attempted; however, in patients with delayed diagnosis and hemorrhagic shock, splenectomy is often the preferable choice.
Methods:
Results:
Conclusion:
Non-traumatic splenic rupture is a rare initial presentation of hematological malignancies. In this case, we present a patient with undiagnosed diffuse large B cell lymphoma who presented to the emergency department with a delayed manifestation of splenic rupture and hemorrhagic shock requiring emergency splenectomy. High level of suspicion and simple bedside imaging methods can be highly sensitive in the diagnosis of non-traumatic splenic rupture. Timely intervention prevents mortality. In a stable patient, splenic salvage may be attempted; however, in patients with delayed diagnosis and hemorrhagic shock, splenectomy is often the preferable choice.
Methods:
Results:
Conclusion:

