General Surgery
Category: Quickshot Oral Session 07
Quickshot Oral : Quickshot Oral Session 07
BONE PIERCING THROUGH THE SUPERIOR MESENTERIC VEIN: A CASE OF FOREIGN BODY MIGRATION
Saturday, February 11, 2023
3:00pm - 4:00pm East Coast USA Time

Dana Nielsen, MD
Resident
University of North Dakota, United States
Dana Nielsen, MD
Resident
University of North Dakota, United States
Presenter(s)
Principal Contact(s)
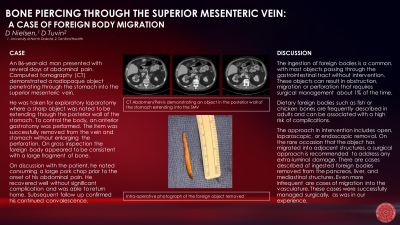
Objectives: Here we describe a case of an 86-year-old man presenting with several days of abdominal pain. Computed tomography (CT) demonstrated a radiopaque object penetrating through the stomach into the superior mesenteric vein with associated thrombus. He was taken for exploratory laparotomy where a sharp object was noted to be extending though the posterior wall of the stomach. To control the body, an anterior gastrotomy was performed. The item was successfully removed from the vein and stomach without enlarging the perforation. There was no hemorrhage noted from the retroperitoneum. On gross inspection the foreign body appeared to be consistent with a large fragment of bone, approximately 45 mm in length. On discussion with the patient, he noted consuming a large pork chop prior to the onset of his abdominal pain. He recovered well without significant complication and was able to return home. Subsequent follow up confirmed his continued convalescence.
This is an 86-year-old man with history of COPD who presented to an outside facility complaining of shortness of breath and increased oxygen requirements. On arrival to that emergency department, he had additionally noted bothersome abdominal pain of several days’ duration and underwent a CT of the abdomen and pelvis. This demonstrated a foreign body in the stomach penetrating the posterior wall into the superior mesenteric vein and he was subsequently transferred to our facility for higher level of management. The surgical oncology team was consulted due the possible need for vein reconstruction, and he proceeded to the operating room for urgent exploration and foreign body removal. A midline laparotomy was performed, and dense adhesions were encountered. These adhesions were lysed, and the inferior border of the stomach was mobilized and the lesser sac entered. There was a gastric perforation on the posterior aspect of the stomach that was closed by a sharp object. To better control the foreign body and retrieve it without enlarging the perforation, a small anterior gastrotomy was made and the foreign body removed. There was no bleeding noted from the retroperitoneum. The gastric perforation was oversewn, and a tongue of omentum was secured to the repair. The gastrotomy was closed in two layers.
He recovered appropriately post-operatively and quickly weaned to his baseline of supplemental oxygen. He was discharged on post-operative day 5 to home with family support. He was seen in surgical oncology clinic and reported good appetite and regular bowel movements.
Methods:
Results:
Conclusion:
This is an 86-year-old man with history of COPD who presented to an outside facility complaining of shortness of breath and increased oxygen requirements. On arrival to that emergency department, he had additionally noted bothersome abdominal pain of several days’ duration and underwent a CT of the abdomen and pelvis. This demonstrated a foreign body in the stomach penetrating the posterior wall into the superior mesenteric vein and he was subsequently transferred to our facility for higher level of management. The surgical oncology team was consulted due the possible need for vein reconstruction, and he proceeded to the operating room for urgent exploration and foreign body removal. A midline laparotomy was performed, and dense adhesions were encountered. These adhesions were lysed, and the inferior border of the stomach was mobilized and the lesser sac entered. There was a gastric perforation on the posterior aspect of the stomach that was closed by a sharp object. To better control the foreign body and retrieve it without enlarging the perforation, a small anterior gastrotomy was made and the foreign body removed. There was no bleeding noted from the retroperitoneum. The gastric perforation was oversewn, and a tongue of omentum was secured to the repair. The gastrotomy was closed in two layers.
He recovered appropriately post-operatively and quickly weaned to his baseline of supplemental oxygen. He was discharged on post-operative day 5 to home with family support. He was seen in surgical oncology clinic and reported good appetite and regular bowel movements.
Methods:
Results:
Conclusion:

