General Surgery
Category: Quickshot Oral Session 07
Quickshot Oral : Quickshot Oral Session 07
A MASSIVE PARA-ESOPHAGEAL HERNIA: AN UNUSUAL CAUSE OF TENSION PHYSIOLOGY LEADING TO CARDIAC ARREST
Saturday, February 11, 2023
3:00pm - 4:00pm East Coast USA Time

Dana Nielsen, MD
Resident
University of North Dakota, United States
Dana Nielsen, MD
Resident
University of North Dakota, United States
Presenter(s)
Principal Contact(s)
Objectives: This is a 28-year-old man with history of super morbid obesity with a body mass index of 81 and a large, Type IV para-esophageal hernia that had been documented two years prior to presentation. He had sought surgical intervention but was advised to lose weight prior to proceeding.
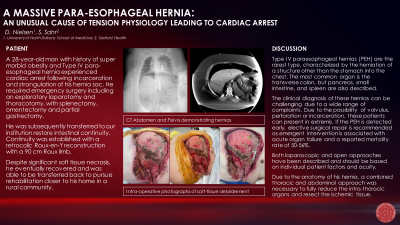
He had noted the sudden onset of severe abdominal pain, nausea and vomiting and subsequently suffered a cardiac arrest in rural Montana. Return of spontaneous circulation was achieved after five rounds of CPR. He was transferred to a local hospital where workup revealed a large, left-sided hemopneumothorax with tension physiology and herniation of abdominal contents into the lateral chest wall. A thoracostomy tube was placed and he was transferred to a higher level of care in Bismarck, ND. At that facility, he was noted to be in severe shock requiring multiple vasopressors. He was taken emergently to the operating room where an exploratory laparotomy with left thoracotomy, splenectomy, omentectomy, partial gastrectomy left in discontinuity and diaphragmatic hernia repair with a left chest wall hernia repair were performed.
He was transferred again to Sanford Medical Center in Fargo due to the anticipated difficulty in restoring intestinal continuity on post-operative day three. He presented intubated and sedated with negative pressure wound therapy over his abdominal and thoracic wounds. He was re-explored on arrival and his remaining viscera was noted to be viable, although with significant loss of domain. He was transferred to the ICU for ongoing resuscitation and on his second procedure at our institution, intestinal continuity was restored with a retrocolic Roux-en-Y reconstruction. A 90 cm Roux limb was fashioned to support weight loss, in accordance with his goals. He required multiple returns to the operating room for serial soft-tissue debridement as the skin and subcutaneous tissue overlying his former hernia necrosed.
His course was complicated by acute kidney failure and he required continuous renal replacement therapy. The tissue loss was significant but eventually stabilized at the level of the intercostal muscles and he was able to transition to negative pressure wound therapy. He was extubated on post-operative day 25 from his index operation. He transitioned to intermittent hemodialysis and started to make some urine. He had return of bowel function and was approved for an oral diet. He was transferred back to Bismarck to begin long-term rehabilitation on post-operative day 33.
Methods:
Results:
Conclusion:
He had noted the sudden onset of severe abdominal pain, nausea and vomiting and subsequently suffered a cardiac arrest in rural Montana. Return of spontaneous circulation was achieved after five rounds of CPR. He was transferred to a local hospital where workup revealed a large, left-sided hemopneumothorax with tension physiology and herniation of abdominal contents into the lateral chest wall. A thoracostomy tube was placed and he was transferred to a higher level of care in Bismarck, ND. At that facility, he was noted to be in severe shock requiring multiple vasopressors. He was taken emergently to the operating room where an exploratory laparotomy with left thoracotomy, splenectomy, omentectomy, partial gastrectomy left in discontinuity and diaphragmatic hernia repair with a left chest wall hernia repair were performed.
He was transferred again to Sanford Medical Center in Fargo due to the anticipated difficulty in restoring intestinal continuity on post-operative day three. He presented intubated and sedated with negative pressure wound therapy over his abdominal and thoracic wounds. He was re-explored on arrival and his remaining viscera was noted to be viable, although with significant loss of domain. He was transferred to the ICU for ongoing resuscitation and on his second procedure at our institution, intestinal continuity was restored with a retrocolic Roux-en-Y reconstruction. A 90 cm Roux limb was fashioned to support weight loss, in accordance with his goals. He required multiple returns to the operating room for serial soft-tissue debridement as the skin and subcutaneous tissue overlying his former hernia necrosed.
His course was complicated by acute kidney failure and he required continuous renal replacement therapy. The tissue loss was significant but eventually stabilized at the level of the intercostal muscles and he was able to transition to negative pressure wound therapy. He was extubated on post-operative day 25 from his index operation. He transitioned to intermittent hemodialysis and started to make some urine. He had return of bowel function and was approved for an oral diet. He was transferred back to Bismarck to begin long-term rehabilitation on post-operative day 33.
Methods:
Results:
Conclusion:

