Colorectal
Category: Quickshot Oral Session 03
Quickshot Oral : Quickshot Oral Session 03
A RARE CASE OF COLORECTAL MALIGNANCY LEADING TO ARTERIOENTERIC FISTULA
Saturday, February 11, 2023
3:00pm - 4:00pm East Coast USA Time
- MK
Matthew Kazaleh, DO
Resident Physician
University of Florida - Jacksonville - GW
Grant Woodruff, DO
United States
Presenter(s)
Principal Contact(s)
Objectives: Arterioenteric fistulas (AEF) are rare and devastating complications of colorectal/pelvic malignancies. The overall incidence of AEF is low, and are exceedingly rare de novo. Unfortunately, these fistulas carry high risk for morbidity and mortality. Here we present a patient who presents in hemorrhagic shock secondary to an advanced colorectal malignancy with local invasion to the right external iliac artery.
Methods: In this case report, we present the complex presentation and management of an AEF. The management involves a multidisciplinary approach, with utmost importance of establishing early goals of care and realistic expectations of outcomes with the patient and family.
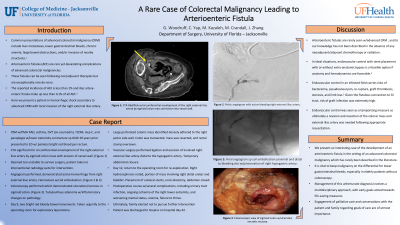
Results: A 70 year old male presented to the emergency department with painless bright red blood per rectum. In the emergency department he was hemodynamically unstable, tachycardic and hypotensive. After obtaining large bore IV access, he was started on immediate blood product resuscitation. NG tube placement with lavage showed no evidence of bleeding, and once stabilized he was transported to CT for imaging. CTA of the abdomen and pelvis was obtained which showed near circumferential envelopment of the right external iliac artery by the sigmoid colon with erosion of the vessel wall. Extensive goals of care discussions were held with the patient and his family. This included the possibility of lower extremity amputation due to vessel involvement with his right external iliac artery. Both the patient and family wished to proceed with all necessary interventions. The patient was too unstable to survive a lengthy abdominal operation, so he was taken to the interventional radiology suite for hemorrhage control. Angiography was obtained which showed active hemorrhage from the right external iliac artery which was coil embolized. He remained hemodynamically stable following intervention, and colonoscopy was obtained several days later, demonstrating multiple polyps and an area of ulceration and necrosis of the sigmoid colon concerning for malignancy. On hospital day 9, he developed more episodes of bright red blood per rectum, and was taken to the operating room for exploration. A partial colectomy, end colostomy and resection of the right external iliac artery was performed. Final pathology showed poorly differentiated colonic adenocarcinoma. He was ultimately discharged to hospice on hospital day 42.
Conclusion: AEF are rare complications of colorectal malignancies. Management of these fistulas involves a multidisciplinary approach. Early engagement with palliative care and communication with the patient and family are equally important for management.
Methods: In this case report, we present the complex presentation and management of an AEF. The management involves a multidisciplinary approach, with utmost importance of establishing early goals of care and realistic expectations of outcomes with the patient and family.
Results: A 70 year old male presented to the emergency department with painless bright red blood per rectum. In the emergency department he was hemodynamically unstable, tachycardic and hypotensive. After obtaining large bore IV access, he was started on immediate blood product resuscitation. NG tube placement with lavage showed no evidence of bleeding, and once stabilized he was transported to CT for imaging. CTA of the abdomen and pelvis was obtained which showed near circumferential envelopment of the right external iliac artery by the sigmoid colon with erosion of the vessel wall. Extensive goals of care discussions were held with the patient and his family. This included the possibility of lower extremity amputation due to vessel involvement with his right external iliac artery. Both the patient and family wished to proceed with all necessary interventions. The patient was too unstable to survive a lengthy abdominal operation, so he was taken to the interventional radiology suite for hemorrhage control. Angiography was obtained which showed active hemorrhage from the right external iliac artery which was coil embolized. He remained hemodynamically stable following intervention, and colonoscopy was obtained several days later, demonstrating multiple polyps and an area of ulceration and necrosis of the sigmoid colon concerning for malignancy. On hospital day 9, he developed more episodes of bright red blood per rectum, and was taken to the operating room for exploration. A partial colectomy, end colostomy and resection of the right external iliac artery was performed. Final pathology showed poorly differentiated colonic adenocarcinoma. He was ultimately discharged to hospice on hospital day 42.
Conclusion: AEF are rare complications of colorectal malignancies. Management of these fistulas involves a multidisciplinary approach. Early engagement with palliative care and communication with the patient and family are equally important for management.

